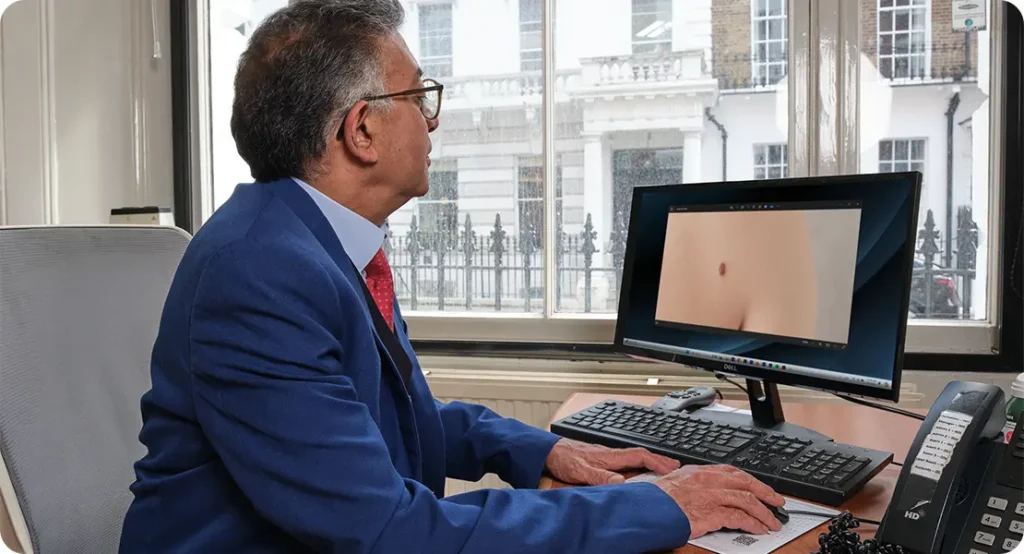
Every skin spot tells a story but deciding which one’s matter, and which ones don’t, is both an art and a science. If you’ve ever visited a dermatologist and wondered how they seem to instantly know whether a rash is harmless or a mole needs a biopsy, you’re not alone. These split-second decisions are the result of years of specialised training, extensive clinical experience, refined pattern recognition, and rigorous evidence-based judgment.
Dermatologists must navigate a complex landscape of symptoms, risk factors, and patient histories, often under time pressure and with significant consequences resting on their choices. Their role requires balancing cautious vigilance with practical efficiency knowing when to reassure patients and when to act decisively. These clinical judgments not only affect immediate treatment plans but can also be pivotal in detecting early signs of skin cancers or rare dermatological diseases. Understanding this decision-making process sheds light on the critical expertise behind every consultation, revealing how dermatologists protect and preserve patients’ health in ways that may not be immediately visible.
What many people may not realise is that dermatology demands continuous learning and adaptability. Skin conditions can mimic one another, evolve over time, and sometimes present with subtle clues that require a keen eye and thoughtful analysis. Every patient encounter is unique, pushing dermatologists to tailor their approach based on the individual’s history, genetics, lifestyle, and even psychological wellbeing. This dynamic and multifaceted nature of dermatological care makes clinical judgement a skill honed over years, blending science, technology, and human insight.
In this article, we’ll walk through the real-world decision-making process dermatologists face daily from how they choose when to monitor versus intervene, to the high-pressure calls they make that can literally save lives. If you’ve ever questioned how much thought goes into a skin exam, this behind-the-scenes look will give you a whole new level of appreciation.
The Quiet Power of Observation

Dermatologists are experts in spotting the smallest signs that something may be wrong tiny shifts in colour, slight changes in texture, irregular borders, or how a lesion reflects light under examination. What might appear minor or unnoticeable to most people can, in the eyes of a dermatologist, signal a deeper concern. These subtle cues often point to potentially serious conditions like melanoma, cutaneous lymphoma, or autoimmune skin disorders. This ability to interpret what others might overlook is one of the quiet, powerful skills that define clinical excellence in dermatology.
During a consultation, your dermatologist may appear to simply be examining your skin but they’re actually applying a complex mental checklist. They’re thinking about:
- Symmetry vs asymmetry
- Evolution of the lesion over time
- Risk factors like sun exposure, immunosuppression, or family history
- Common vs rare presentation patterns
Each of these observations helps form an internal risk profile, and the stakes are high. Missing a dangerous lesion can delay treatment, but biopsying everything unnecessarily causes scarring, anxiety, and healthcare strain. It’s all about finding that delicate balance.
When to Reassure and When to Biopsy
Few decisions in dermatology carry more weight than choosing between reassurance and action. Knowing when to say, “This looks harmless, no treatment needed,” versus “We should biopsy this to be safe,” requires not just training, but clinical confidence built over years. Reassurance needs to be well-grounded based on solid pattern recognition, risk assessment, and diagnostic tools. On the other hand, recommending a biopsy must be timely, precise, and supported by a clear rationale. It’s this constant balance between avoiding unnecessary procedures and catching serious conditions early that defines the art of dermatological judgement.
Biopsy decisions hinge on:
- The lesion’s appearance under dermoscopy
- Patient history and symptom description
- How the lesion compares to others on the body
- Whether it has changed recently or appeared suddenly
This is where clinical judgment really matters. Dermatologists are constantly weighing risks: Is this mole just atypical, or is it evolving into something malignant? Should I wait and monitor it, or remove it now?
The Pressure of Not Missing a Diagnosis
In dermatology, where so much relies on visual examination, the fear of missing a diagnosis is very real. A single overlooked skin cancer can have life-altering consequences for the patient and leave a lasting emotional toll on the physician. That’s why dermatologists are trained to walk a fine line: staying alert to subtle warning signs without overreacting to every harmless spot. It’s a skill rooted in both caution and clinical pragmatism.
To stay ahead, dermatologists constantly review guidelines, seek second opinions for ambiguous cases, and rely on tools like dermoscopy to improve diagnostic accuracy. Their decisions are rarely rushed each one carries the weight of protecting lives.
They’re often navigating:
- The fear of patient litigation if something is missed
- Avoiding over-biopsying benign lesions that could cause unnecessary harm
- Trusting instinct without relying solely on it
- Balancing clinical expertise with diagnostic tools like dermoscopy, AI imaging, or total body photography
This daily tension means dermatologists must stay sharp, updated, and constantly reflective in their decision-making process. Every diagnosis is an opportunity to learn, and every patient encounter reinforces the delicate balance between caution and confidence. Peer discussions, multidisciplinary case reviews, and professional development are not just optional they’re essential practices for maintaining accuracy and excellence. In a field where small oversights can lead to serious outcomes, the commitment to ongoing vigilance isn’t just professional it’s deeply personal.
Using Dermoscopy and Imaging as Diagnostic Allies
Technology is playing an increasingly vital and transformative role in enhancing clinical judgment within dermatology. Advanced diagnostic tools such as dermoscopes, reflectance confocal microscopy, and AI-powered diagnostic software are revolutionizing the way skin lesions are evaluated and interpreted. These innovations provide dermatologists with critical insights that go far beyond what the naked eye can discern, enabling earlier and more accurate diagnoses.
A dermatoscope, for instance, is an essential handheld device that allows the dermatologist to examine skin lesions at a magnified level, revealing intricate details like pigment networks, blood vessel arrangements, and other microscopic structures that are invisible during a routine visual exam. When used correctly, dermoscopy significantly improves diagnostic accuracy, helping clinicians differentiate benign moles from potentially malignant ones, and thereby reducing the number of unnecessary biopsies and surgical procedures. This not only benefits patients by minimizing invasive interventions but also helps optimize healthcare resources.
In addition to dermoscopy, digital technologies such as high-resolution photography, total body mapping, and mole tracking software provide invaluable support in monitoring changes in suspicious lesions over time. These tools are especially useful for patients with multiple moles or those at elevated risk of melanoma due to family history or genetic predisposition. By capturing precise images during regular check-ups, dermatologists can detect subtle changes that might indicate malignancy at an earlier stage.
Communication: A Critical Clinical Skill
Making high-stakes clinical decisions in dermatology isn’t just about accurately diagnosing skin conditions it’s equally about how those decisions are communicated to the patient. Effective communication is a vital skill for dermatologists, who must clearly and compassionately convey complex information. Whether they are reassuring a patient that a rash is harmless or preparing them for the possibility of a biopsy, the way this information is shared can significantly impact a patient’s understanding, comfort, and trust. It’s important to explain:
- Why a biopsy may or may not be necessary, helping patients understand the rationale behind the recommendation.
- What the biopsy procedure will involve, including what they can expect during and immediately after the process.
- The possible outcomes of the biopsy, including both benign and serious results, and how these results will guide further care.
- When patients can expect to receive their biopsy results, as well as the likely next steps depending on those outcomes.
Many patients come into skin consultations carrying emotional burdens whether from a personal or family history of skin cancer, previous scarring, or ongoing chronic skin conditions. Recognizing and addressing these concerns with empathy is essential. A calm, informative, and supportive conversation can greatly alleviate patient anxiety, build confidence, and foster a collaborative approach to their care.
How Experience and Specialisation Shape Judgment
Not all dermatologists approach clinical decisions in the same way and that diversity is actually a strength within the field. For example, a dermatologist who specialises in skin cancer may have a much lower threshold for recommending a biopsy, prioritising early detection and aggressive intervention. In contrast, a paediatric dermatologist might lean more towards careful observation and watchful waiting, recognising that many childhood skin conditions resolve on their own or behave differently than in adults. These varying approaches reflect the nuances of specialisation and the tailored care needed for different patient groups.
Over years of clinical practice, experience profoundly sharpens a dermatologist’s pattern recognition skills and helps develop what is often described as clinical intuition or “gut feeling.” This refined judgment is built on countless patient encounters, exposure to rare cases, and continuous learning, enabling dermatologists to quickly differentiate between routine conditions and those that require urgent attention.
However, even the most seasoned specialists do not rely solely on intuition. Complex or ambiguous cases are frequently reviewed in multidisciplinary team meetings or discussed with colleagues to ensure the best possible outcomes. Dermatologists also use diagnostic algorithms, clinical guidelines, and the latest evidence-based research to ground their decisions in scientific rigor rather than personal bias or ego. This collaborative, thoughtful approach ensures that patient care remains safe, effective, and responsible balancing experience with continual learning and teamwork.
Biopsy Is Not Always the End of the Story
Even after a biopsy, the decision-making process for dermatologists is far from over. They must carefully review the biopsy results to determine whether the diagnosis is definitive or if further testing is necessary. Questions arise such as: Was the biopsy taken from the most representative area of the lesion? Are the surgical margins clear, or is there a need to extend them? Depending on the findings, dermatologists may need to refer the patient to oncology for cancer treatment or to plastic surgery for reconstructive procedures.
Dermatology is a field full of moving parts the initial biopsy may provide clear answers, or it could be just the beginning of a more complex investigation. What follows is a series of ongoing judgments, monitoring, and adjustments to the treatment plan, all aimed at ensuring safe and effective patient care.
Key Points to Remember:
- Biopsies provide critical information but must be interpreted within the broader clinical context.
- Follow-up care and reassessment are essential to address evolving or persistent skin issues.
- Collaboration with other specialists often plays a crucial role in managing complex or serious conditions.
Frequently Asked Questions (FAQ)
- What is a dermatological biopsy, and when is it needed?
A biopsy involves removing a small piece of skin tissue to examine under a microscope. Dermatologists recommend it when a lesion looks suspicious, unclear, or rapidly changing. It helps confirm diagnoses like skin cancer, infections, or inflammatory conditions. - How do dermatologists decide whether to biopsy a lesion or not?
They use a combination of visual cues, dermoscopy, patient history, and clinical experience. They weigh factors like lesion symmetry, colour variation, border irregularity, and recent changes to make that call. The goal is to balance safety with avoiding unnecessary procedures. - Can skin cancer be diagnosed without a biopsy?
Sometimes, but not definitively. A dermatologist might suspect skin cancer based on clinical appearance and dermoscopy, but a biopsy is typically required for confirmation. It’s the most reliable method to determine if a lesion is benign or malignant. - Is it possible for a dermatologist to miss something serious?
While dermatologists are trained to catch subtle warning signs, like any specialty, no diagnostic process is perfect. That’s why they use tools like dermoscopy, AI imaging, and follow-up reviews to minimise the chance of missed diagnoses. - What should I do if I feel uncertain after a skin check?
Always feel empowered to ask questions or seek a second opinion. You can ask your dermatologist to explain their reasoning or monitor the lesion over time. Open communication helps build trust and ensures you stay actively involved in your care. - What happens if a biopsy comes back inconclusive?
Sometimes, a biopsy may not give a clear diagnosis this is called an inconclusive or non-specific result. In such cases, your dermatologist may recommend a follow-up biopsy, refer you for additional testing, or closely monitor the area over time. It’s not uncommon and doesn’t automatically mean something serious, but it does require careful follow-up to ensure nothing is missed. - How long does it take to get biopsy results from a dermatologist?
Biopsy results usually take 5 to 10 working days, depending on the type of analysis required. In urgent cases, results may be expedited. Your dermatologist will inform you when to expect the outcome and schedule a follow-up to discuss it. They’ll also explain the findings in simple terms and walk you through any next steps if treatment or further testing is needed. - Is every mole or skin spot a potential cancer risk?
Not at all. Most moles and skin spots are completely benign and pose no health risk. However, changes in size, colour, border, or shape or the sudden appearance of new lesions can be signs worth checking. Dermatologists use tools like dermoscopy and clinical history to distinguish harmless growths from those that may need further investigation. Regular skin checks and self-monitoring help catch issues early, long before they become serious.
Final Thoughts: When Skin Decisions Save Lives
Each day, dermatologists navigate the delicate balance between caution and precision in their clinical judgments. They are far more than just experts in skin health they are highly skilled decision-makers who integrate medical science, patient history, advanced technology, and clinical intuition to deliver the best possible care. This complex interplay ensures that even the smallest skin changes are carefully assessed, making their role vital in detecting serious conditions early and ultimately saving lives.
If you’re ever unsure about a lesion or a diagnosis, don’t hesitate to ask your dermatologist how they reached their decision. Their thought process is likely more detailed and deliberate than you imagined. If you’re looking for clarity or guidance, don’t hesitate to book a consultation with one of our experienced dermatologists, who will carefully evaluate every sign, symptom, and subtle change to provide you with the best care.
References:
- Marks, R., 2020. Dermoscopy and skin cancer: A practical guide. 2nd ed. Oxford: Wiley-Blackwell.
- Rosendahl, C., Tschandl, P., Cameron, A. and Kittler, H., 2019. Diagnostic accuracy of dermatoscopy: a meta-analysis. British Journal of Dermatology, 180(2), pp.250–257. Available at: https://doi.org/10.1111/bjd.17266[Accessed 5 Jun. 2025].
- British Association of Dermatologists (BAD), 2023. Skin biopsy procedures: Clinical guidelines. [online]
- American Academy of Dermatology (AAD), 2023. Approach to skin lesion assessment. [online] Available at: https://www.aad.org/member/clinical-quality/clinical-care [Accessed 5 Jun. 2025].
- National Institute for Health and Care Excellence (NICE), 2022. Skin cancer – recognition and referral (NG12). [online] Available at: https://www.nice.org.uk/guidance/ng12 [Accessed 5 Jun. 2025].
