If your skin stings when you apply moisturiser, reacts to cold wind, or flares up after trying a new product, you’re not alone. Sensitive skin is one of the most common complaints in dermatology and one of the most misunderstood.
Many people assume sensitivity simply means “dry skin.” But in reality, it can signal deeper issues such as rosacea, eczema, or contact dermatitis, or result from a weakened skin barrier that needs professional attention.
In this article, we’ll explore what truly causes sensitive skin, when it’s a sign of something more serious, and how a dermatologist can help you find lasting relief rather than just temporary fixes.
What Does “Sensitive Skin” Really Mean?
“Sensitive skin” isn’t a medical diagnosis. It’s a broad term describing skin that reacts easily to external or internal triggers such as cosmetics, temperature changes, or even stress.
You may experience:
- Burning or stinging sensations
- Redness or flushing
- Tightness, dryness, or itching
- Visible irritation after applying skincare products
These symptoms suggest your skin’s protective barrier isn’t functioning properly. That barrier is meant to keep moisture in and irritants out but when it weakens, even mild products or normal conditions can cause discomfort.
Common Triggers of Sensitive Skin
While everyone’s triggers are unique, some culprits are especially common:
1. Harsh Skincare Ingredients
Fragrance, alcohol, sulphates, and acids (like glycolic or salicylic) can irritate compromised skin.
2. Over-Exfoliation
Too many scrubs or peels strip the barrier, leading to inflammation and dryness.
3. Environmental Factors
Cold weather, pollution, and low humidity reduce hydration and increase irritation.
4. Stress and Hormones
Stress hormones like cortisol can increase skin inflammation and sensitivity.
5. Medical Conditions
Skin sensitivity can also stem from conditions such as eczema, rosacea, seborrhoeic dermatitis, or allergic contact dermatitis all of which require professional diagnosis and treatment.
When Sensitive Skin Signals a Deeper Issue
Occasional irritation is normal, but if your symptoms persist or worsen despite gentle care, your skin could be reacting to an underlying dermatological condition.
Here are a few that commonly present as “sensitive skin”:
1. Rosacea
Rosacea often starts with frequent flushing or redness on the cheeks, nose, or forehead. Over time, small visible blood vessels (telangiectasia) and bumps can appear.
If your skin burns or turns red easily, particularly after heat, alcohol, or spicy food, rosacea may be the cause.
How a dermatologist can help:
- Prescription anti-inflammatory creams or oral antibiotics.
- Laser or light-based therapies to reduce redness.
- Lifestyle advice on avoiding known triggers.
2. Eczema (Atopic Dermatitis)
Eczema involves a weakened skin barrier and overactive immune response. It causes dry, itchy patches that can crack and bleed.
It often flares with stress, allergies, or changes in temperature. In adults, it can appear on the face, hands, or neck.
How a dermatologist can help:
- Medical-grade moisturisers and steroid or non-steroid creams.
- Identifying allergen or irritant triggers.
- Advice on long-term skin barrier repair and hydration.
3. Contact Dermatitis
This form of dermatitis occurs when your skin reacts to a particular substance like perfume, metal, or a skincare ingredient.
Two types exist:
- Irritant contact dermatitis a direct reaction to a harsh substance.
- Allergic contact dermatitis an immune response triggered by exposure to a specific allergen.
How a dermatologist can help:
- Patch testing to identify specific allergens.
- Tailored treatment and avoidance plan.
- Prescription creams to reduce inflammation.
4. Seborrhoeic Dermatitis
This condition causes flaky, red patches around the nose, eyebrows, or scalp. It’s often mistaken for dry skin, but it’s actually linked to an overgrowth of a natural skin yeast (Malassezia).
How a dermatologist can help:
- Anti-fungal or medicated shampoos.
- Mild steroid or anti-inflammatory creams.
- Lifestyle and skincare advice to manage flare-ups.
The Role of the Skin Barrier
At the root of nearly all sensitive skin issues lies a compromised skin barrier the thin layer of lipids and cells that protects you from external stressors.
When the barrier weakens, water escapes easily (causing dryness) and irritants penetrate more easily (causing inflammation).
What damages the barrier:
- Over-cleansing or using foaming soaps.
- Harsh exfoliation or strong acids.
- Overuse of retinol without tolerance building.
- Sudden changes in climate or humidity.
How to support your barrier:
- Choose gentle, pH-balanced cleansers.
- Moisturise regularly with ceramide-rich creams.
- Avoid unnecessary actives until your skin stabilises.
Think of barrier care as rebuilding your skin’s armour it’s the foundation for every other skin treatment.
Ingredients That Often Worsen Sensitive Skin

If your skin tends to react easily, it’s important to know which ingredients can make things worse. Here are some of the most common irritants to watch out for:
Fragrance:
Perfumes and essential oils might smell lovely, but they’re among the biggest culprits behind allergic reactions and flare-ups. If your skin is sensitive, even a small amount can trigger redness or itching.
Alcohols:
Ingredients like ethanol or SD alcohol can dry out the skin and cause that uncomfortable stinging sensation. They strip away natural moisture, leaving your barrier even more vulnerable.
Acids:
Exfoliating acids such as glycolic, lactic, and salicylic acid can be too harsh for delicate skin. While they help resurface and brighten, overuse can lead to irritation and inflammation.
Preservatives:
Compounds like methylisothiazolinone and parabens are used to extend a product’s shelf life, but they’re also known to cause contact dermatitis in sensitive individuals.
Synthetic dyes:
These are often added to make cosmetics look more appealing, but artificial colourants can inflame sensitive skin and cause unwanted reactions.
When in doubt, reach for products labelled “fragrance-free”, “hypoallergenic”, or “dermatologist-tested.” These are formulated with fewer irritants and are generally gentler on reactive skin.
The Importance of pH Balance
Healthy skin has a slightly acidic pH (around 4.5–5.5). This acidity helps protect against bacteria and supports the lipid barrier.
Using cleansers or toners that are too alkaline disrupts this balance, leading to irritation and dryness.
Opt for mild, soap-free formulas that cleanse without stripping your natural oils.
How to Build a Gentle Skincare Routine
Sensitive skin thrives on simplicity. Here’s a dermatologist-approved structure:
1. Cleanse (AM/PM)
Use a mild, creamy cleanser that doesn’t foam. Avoid exfoliating beads or acids.
2. Moisturise (AM/PM)
Apply a fragrance-free moisturiser containing:
- Ceramides: to strengthen the barrier.
- Niacinamide: to calm redness and improve resilience.
- Glycerin or hyaluronic acid: to attract water.
3. Protect (Morning)
Always wear SPF 30+ daily, even when indoors. Sensitive skin is often more prone to sun-induced inflammation and pigmentation.
4. Repair (Evening)
At night, use a barrier-repair balm or cream with panthenol or squalane.
5. Optional: Targeted Treatments
If prescribed by your dermatologist, include mild anti-inflammatory or soothing serums but avoid layering too many products.
Less is more when calming reactive skin.
Lifestyle Habits That Help Sensitive Skin
1. Manage Stress
Stress can release cortisol, worsening inflammation and rosacea. Try yoga, walking, or breathing exercises.
2. Watch Your Diet
Spicy foods, caffeine, and alcohol can trigger flushing in sensitive or rosacea-prone skin. Balance these with anti-inflammatory foods rich in omega-3 and antioxidants.
3. Sleep Well
Sleep supports the skin’s nightly repair cycle. Aim for 7–8 hours to reduce inflammation and dark circles.
4. Humidify Your Space
Indoor heating and air conditioning strip air moisture. A humidifier restores balance, preventing dryness and irritation.
5. Avoid Hot Showers
Use lukewarm water to avoid stripping natural oils.
When to See a Dermatologist
You should see a dermatologist if:
- Your skin stings or burns with almost any product.
- Redness, flaking, or bumps persist for more than two weeks.
- You suspect eczema, rosacea, or contact dermatitis.
- Over-the-counter products provide little or no relief.
- You notice sudden changes in sensitivity without clear reason.
A dermatologist can conduct patch tests, assess your skin barrier, and tailor a skincare or prescription plan that truly calms your skin.
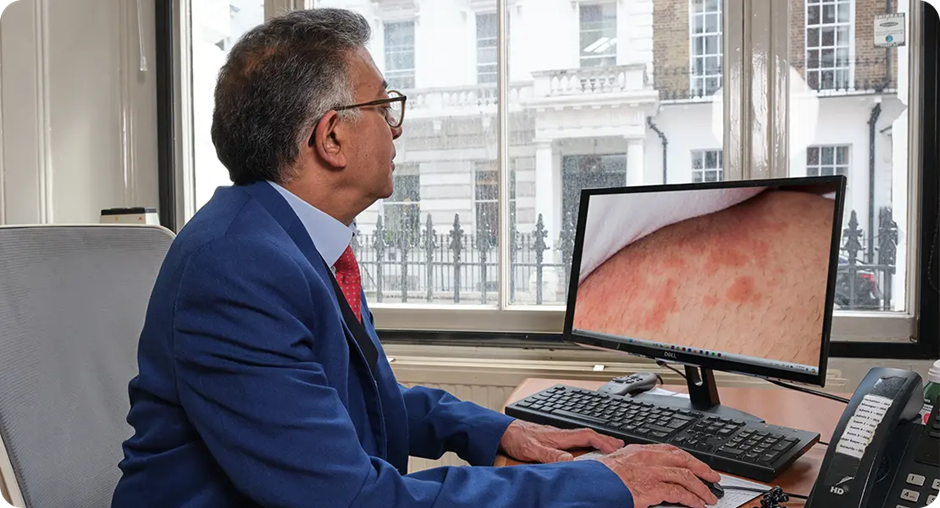
How Dermatologists Treat Sensitive Skin
1. Patch or Allergy Testing
Identifies whether an allergen or irritant ingredient is behind your reactions.
2. Topical Medications
Includes anti-inflammatory creams, barrier-repair formulations, or topical antibiotics (for rosacea).
3. Oral Medications
For severe cases, antibiotics or low-dose anti-inflammatories may be prescribed to control flare-ups.
4. In-Clinic Treatments
- LED light therapy: reduces inflammation and redness.
- Laser therapy: targets visible veins or rosacea-related flushing.
- Hydrating facials: restore moisture safely with medical-grade serums.
5. Long-Term Skin Health Plans
A dermatologist doesn’t just treat flare-ups they create a sustainable care plan that keeps your skin calm, balanced, and resilient.
Signs You Might Be Over-Treating Your Skin
In today’s world of 10-step routines and constant product launches, over-treatment is a common cause of sensitivity.
You may be overdoing it if you notice:
- Burning after applying skincare.
- Constant dryness or flaking.
- Tightness despite moisturising.
- Sudden breakouts or redness after layering products.
Simplify your regimen for a few weeks and let your skin recover. Sometimes, healing means doing less.
Sensitive Skin vs Allergic Skin: The Difference
It’s easy to mix up sensitive skin with allergic skin after all, both can leave you red, itchy, and uncomfortable. But the causes (and solutions) are actually quite different.
Sensitive skin reacts to general irritants such as fragrance, harsh weather, or even stress. The reaction tends to happen quickly you might feel redness, stinging, or burning right after using a product but it usually fades once the trigger is removed. This kind of reaction often comes from a weakened skin barrier or ongoing inflammation. Strengthening that barrier with gentle, hydrating care is the key to keeping sensitivity under control.
Allergic skin, on the other hand, reacts to specific substances your immune system sees as threats things like nickel, preservatives, or certain cosmetic ingredients. The tricky part is that these reactions don’t always appear right away. Sometimes, redness, swelling, or itching can show up hours or even days later. Managing allergic skin is all about identifying and avoiding the exact allergen causing the response.
If you’re not sure which category you fall into, it’s best to get a patch test from a dermatologist. It can pinpoint what’s really behind your skin’s reactions and help you find products that work safely for you.
Choosing the Right Products for Sensitive Skin
When shopping for skincare, keep these principles in mind:
1. Less is more. Choose multi-purpose products instead of layering many.
2. Fragrance-free, not unscented. “Unscented” can still contain masking agents.
3. Creams over lotions. Creams contain more emollients, sealing moisture better.
4. Check expiry dates. Expired products may irritate even healthy skin.
5. Patch-test new products. Apply a small amount behind your ear for 48 hours before full use.
Sensitive Skin During Seasons
Winter:
Cold air and indoor heating can cause dryness. Use heavier moisturisers and avoid long, hot showers.
Summer:
Sweat and sun can trigger irritation. Opt for lightweight SPF moisturisers and gentle cleansing.
Spring/Autumn:
Pollen and temperature swings may worsen redness or flare-ups keep calming sprays or barrier creams on hand.
Adjusting your skincare seasonally can prevent many sensitivity-related flare-ups.
Why Self-Diagnosis Can Be Risky
Because sensitive skin has so many causes, self-diagnosing can lead to using the wrong products or making things worse.
For example:
- Someone with rosacea may try exfoliating acids for texture, worsening redness.
- A person with eczema may use rich oils that trap heat and aggravate inflammation.
Only a qualified dermatologist can identify what’s really happening beneath the surface and tailor a plan that works safely for you.
Frequently Asked Questions About Sensitive Skin:
1. How do I know if I have sensitive skin or just dry skin?
Dry skin simply lacks moisture, which can make it feel tight or flaky. Sensitive skin, however, goes beyond dryness it reacts easily to products, temperature changes, or even stress. If your face stings or turns red after applying moisturiser or being exposed to wind, that’s a sign of sensitivity rather than just dryness.
2. Can sensitive skin suddenly develop in adulthood?
Yes, sensitivity can appear later in life even if your skin was once resilient. Hormonal changes, prolonged use of strong actives, pollution, stress, or a weakened skin barrier can all make your skin more reactive over time. It’s not unusual for people in their 30s or 40s to notice new triggers they never had before.
3. What’s the best way to calm my skin during a flare-up?
When irritation hits, the first step is to strip back your routine. Avoid exfoliants, retinoids, and fragrances for at least a few days. Use a mild, fragrance-free cleanser and a ceramide-rich moisturiser to soothe the barrier. Applying a cool, damp cloth for a few minutes can also reduce burning and redness. And of course, resist the urge to try new products until your skin settles.
4. Are natural or organic products better for sensitive skin?
Not necessarily. While “natural” sounds gentler, many botanical extracts and essential oils can actually cause irritation or allergic reactions. What matters more is the formulation look for simple, fragrance-free products with minimal ingredients. Even a laboratory-made moisturiser can be safer than a natural one packed with reactive plant oils.
5. Can stress really make sensitive skin worse?
Absolutely. Stress triggers the release of cortisol, a hormone that weakens the skin barrier and increases inflammation. When cortisol levels stay high, your skin becomes more prone to redness, itching, and flare-ups. Managing stress through sleep, exercise, or mindfulness isn’t just good for your mind it’s vital for calmer, healthier skin.
6. Is sunscreen safe for sensitive skin?
Yes, but choose wisely. Chemical sunscreens can sometimes sting or irritate, while mineral-based formulas with zinc oxide or titanium dioxide are generally more soothing. Look for a lightweight, fragrance-free SPF 30 or higher that’s labelled for sensitive skin. Remember, skipping sunscreen can actually worsen sensitivity by exposing fragile skin to UV damage.
7. How long does it take to repair a damaged skin barrier?
It depends on how compromised your skin is. Mild barrier irritation may recover within a week of using gentle, hydrating products. But if your barrier is severely weakened from over-exfoliation or harsh treatments it can take several weeks to fully restore. Consistency is key: stick with nourishing moisturisers, avoid active ingredients, and keep your routine minimal.
8. Can sensitive skin still use actives like retinol or vitamin C?
Yes, but with caution. You can introduce actives slowly once your barrier feels strong again. Start with low concentrations, apply every few nights, and always follow with a soothing moisturiser. Buffered or encapsulated formulas tend to be less irritating. If redness or stinging returns, pause and let your skin recover before trying again.
9. Should I see a dermatologist if my sensitivity keeps coming back?
Definitely. Persistent sensitivity could signal something more complex, such as rosacea, eczema, or allergic contact dermatitis. A dermatologist can perform patch tests, identify the root cause, and prescribe treatments that target the problem instead of just masking the symptoms. Professional advice saves time, money, and further irritation.
10. What’s one common mistake people make with sensitive skin?
The biggest mistake is assuming more products mean better results. Overloading your routine with multiple serums, exfoliants, and masks often backfires. Sensitive skin thrives on simplicity. Fewer, well-chosen products that focus on hydration and barrier repair will always outperform a complicated routine.
Final Thought: Getting to the Root of Skin Sensitivity
Sensitive skin can feel unpredictable, but it’s not something you have to live with forever. Whether your irritation stems from a weak skin barrier, an underlying condition like rosacea or eczema, or reactions to everyday ingredients, understanding your triggers is the first step toward calmer, healthier skin.
If you’ve already tried simplifying your routine and the redness or stinging persists, it’s time to get professional help. A dermatologist can pinpoint the root cause of your sensitivity, recommend the safest treatment plan, and help rebuild your skin’s resilience with medical-grade care. If you would like to book a consultation with one of our dermatologists, you can contact us at the London Dermatology Centre.
References:
1. Duarte, I., Silveira, J.E.P.S., Hafner, M.F., Toyota, R. & Pedroso, D.M.M., 2017. Sensitive skin: review of an ascending concept. Anais Brasileiros de Dermatologia, 92(4), pp.620-621. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5595600/
2. Baker, P., 2023. Skin barrier function: the interplay of physical, chemical and microbial factors. Journal of Dermatological Science, 110, p.103. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10706187/
3. Farage, M.A., 2021. Understanding the sensitive skin subject to achieve a more holistic diagnosis. Cosmetics, 8(3), 81. Available at: https://www.mdpi.com/2079-9284/8/3/81
4. Wu, Y., 2021. Compromised skin barrier and sensitive skin in diverse populations. Journal of Drugs in Dermatology Online, 20(4), pp. S154-S159. Available at: https://europepmc.org/article/med/33852256
5. “Mechanisms of Sensitive Skin and the Soothing Effects of Active Ingredients.” 2023. Cosmetics, 11(6), 190. Available at: https://www.mdpi.com/2079-9284/11/6/190
