If you’ve ever wished for more effective ways to treat stubborn scars, 2026 is shaping up to be one of the most exciting years in dermatology. The world of scar treatment is evolving quickly, and the technologies emerging now promise better results, faster healing and more personalised treatment options than ever before. Whether you’re dealing with acne scars, surgical scars, injury scars or stretch marks, new innovations are offering hope for smoother, healthier-looking skin.
As dermatologists gain access to smarter lasers, regenerative injectables, biological topicals and enhanced radiofrequency devices, the options for treating scars are expanding dramatically. These new treatments focus not just on resurfacing the skin but on understanding how scars behave beneath the surface. The goal is to remodel scar tissue more deeply, regenerate healthier collagen and restore a more natural texture.
In this guide, I’ll take you through the most promising developments expected to define scar treatment in 2026. I’ll explain how these technologies work, which types of scars they help most and why this year is a turning point in the field of scar revision.
Why Scar Treatment Is Changing So Quickly
Scar treatment has historically focused on resurfacing the top layer of the skin. While older techniques helped smooth irregularities, they didn’t always address the deeper layers where scar tissue forms. Over time, dermatology has shifted towards stimulating regeneration at a cellular level. This means repairing scar structure rather than simply removing or flattening the surface.
New research into wound healing, fibroblast behaviour, collagen remodelling and controlled inflammation has helped scientists create devices and treatments that work with your skin’s natural biology. Instead of forcing the skin to change through damage, modern treatments encourage healthier tissue to replace scar tissue from within.
This shift has paved the way for more advanced and more personalised options, many of which you’ll see widely available in 2026.
The Rise of Regenerative Dermatology

Regenerative medicine has influenced scar treatment significantly. Instead of focusing solely on resurfacing, treatment now involves stimulating your own body to rebuild damaged collagen and elastin. This new direction allows for better results on stubborn and older scars that previously responded poorly to resurfacing alone.
Why Regeneration Matters
- Deep tissue renewal – Regenerative treatments rebuild collagen at the foundation level, improving thickness, texture and long-term scar appearance.
- More natural results – Because your own tissue is restored gradually, your outcome looks smooth and blends seamlessly with surrounding skin.
- Better tolerance – Regenerative therapies often involve less downtime and fewer side effects compared to older resurfacing technologies.
This movement is reshaping how scars are treated across all skin types.
Innovation #1: Next-Generation Fractional Lasers
Fractional lasers have been a cornerstone of scar treatment for over a decade, but the models emerging in 2026 offer unprecedented precision. These devices don’t just deliver energy into the skin they adapt to your scar’s depth, density and thickness using real-time feedback technology. They map scar tissue in microscopic detail and then adjust energy delivery dynamically.
This allows dermatologists to treat raised, indented and mixed-type scars more accurately than ever before. New scanners also improve comfort by distributing energy more evenly, which helps reduce recovery time.
Key Advancements in 2026
- AI-guided energy control – Lasers can now adjust power, depth and density automatically based on your skin’s response.
- Dual-wavelength capability – These systems target both superficial irregularities and deeper scar tissue in one treatment.
- Improved healing response – Faster epithelial repair means a gentler recovery with better overall texture improvement.
Fractional lasers remain a top choice for acne scars, surgical scars and long-standing indentations.
Innovation #2: Topical Biologics That Reprogram Scarring
Biologics are one of the most exciting developments for 2026. These new topicals contain peptides, growth factors and exosome-derived molecules that help control how the skin heals. Instead of waiting until a scar develops, these biologics intervene during the healing stage to prevent excess collagen build-up and abnormal tissue formation.
They are especially promising for fresh surgical scars, traumatic injuries and inflammatory acne lesions that risk turning into long-term marks.
What Makes Biologics Powerful
- Cell-signalling ability – They influence fibroblasts the key cells responsible for collagen helping them create smoother, organised tissue.
- Prevention-focused – Used early, they can reduce scar thickness and pigmentation before it becomes established.
- Compatibility – Biologics work well alongside lasers, RF microneedling and chemical treatments, enhancing overall results.
This category represents a major leap forward in early scar management.
Innovation #3: Enhanced RF Microneedling Devices
RF microneedling has already transformed scar treatment by combining controlled injury with deep thermal stimulation, but the 2026 upgrades take it a step further. New devices deliver energy more uniformly and penetrate deeper layers with greater precision. They also feature smarter needle-tips that adapt to different scar types within the same session.
For people with pitted acne scars, rolling scars or tethered scars, this enhanced precision makes a dramatic difference.
Why RF Is Evolving
- Depth control upgrades – Needles now adjust depth dynamically, ensuring optimal impact across uneven scar patterns.
- Higher energy stability – Improved thermal delivery helps remodel even thicker scar tissue.
- Less surface trauma – Better insulation lowers redness and downtime compared to older systems.
RF microneedling remains one of the most versatile treatments for mixed acne scarring.
Innovation #4: Injectable Regenerative Therapies
2026 introduces a new wave of regenerative injectables designed specifically for scar tissue. These treatments differ from dermal fillers because they don’t work by adding temporary volume. Instead, they encourage long-term collagen and extracellular matrix repair.
Some injectables are derived from poly-L-lactic acid (PLLA) technology, similar to products used for facial rejuvenation. Others are based on regenerative proteins or modified hyaluronic formulations that focus on improving tissue quality rather than filling indentations superficially.
Key Strengths of Regenerative Injectables
- Deep collagen activation – They stimulate new tissue formation around the scar, improving texture and firmness.
- Long-term change – Results last months to years because they modify tissue rather than simply filling it.
- Targeted application – Ideal for indented acne scars, atrophic scars and areas with volume deficit.
These injectables complement other modalities and make scar treatment more customisable.
Innovation #5: Laser-RF Hybrid Devices
One of the most anticipated scar treatment innovations for 2026 is the rise of hybrid platforms that combine fractional laser energy with radiofrequency microneedling in a single system. This dual action allows dermatologists to address both the surface irregularities and deeper fibrotic bands within a scar during the same session.
The synergy of heat, mechanical breakdown and resurfacing leads to faster improvement with fewer treatment appointments.
Hybrid devices are especially helpful for acne scars that involve multiple layers of irregularity.
Innovation #6: Collagen-Modulating Light Therapies
Low-level light therapy (LLLT) and LED systems have existed for many years, but 2026 models feature advanced wavelengths designed specifically for modulating scar formation. These lights influence cellular metabolism, reduce inflammation and improve collagen architecture.
They are gentle enough for sensitive skin and ideal as a secondary treatment following lasers or microneedling. Patients with pigmentation concerns may also benefit because certain wavelengths help regulate melanin activity.
Innovation #7: Scar-Specific Ultrasound Tightening
Ultrasound devices for skin tightening have traditionally been used in anti-ageing treatments, but new versions are emerging that specifically target scar firmness and tension. These devices deliver focused ultrasound energy into deep layers of scar tissue, helping to soften tight, restrictive areas.
This technology is particularly effective for surgical scars and traumatic scars that restrict movement or feel rigid.
Which Scars Benefit Most From These Innovations?
Advances in scar treatment now allow dermatologists to target specific aspects of scar formation. The best results are achieved when the treatment is carefully matched to the scar type, rather than relying on a single approach.
Scar Types and Best Treatments
- Indented acne scars
These respond well to RF (radiofrequency) microneedling, hybrid devices, and regenerative injectables. These treatments stimulate collagen production and lift depressed areas, improving texture and overall appearance. - Raised surgical scars
Biologics, fractional lasers, and ultrasound-based softening techniques help flatten and soften elevated scars. They reduce stiffness and redness while promoting smoother, more natural skin. - Fresh wounds at risk of scarring
Early intervention with topical biologics can guide healing and prevent severe scar formation. Applying the right therapy during the initial healing stage can minimise long-term discoloration and texture changes.
Matching the right treatment to the specific scar type leads to better outcomes, faster improvement, and more natural-looking skin.
Combination Therapy: The Real Future of Scar Treatment
While individual innovations in scar care are impressive on their own, the greatest improvements come from combination treatments. Dermatologists have found that layering therapies yields better results because it targets multiple aspects of scar formation simultaneously. In 2026, clinics are expected to use sophisticated treatment plans involving lasers, biologics, RF microneedling, and regenerative injectables, applied in carefully timed intervals for maximum effectiveness.
Why Combination Therapy Works
- Multi-layer repair
Scars affect the epidermis, dermis, and sub-dermal layers. Combination therapy allows dermatologists to treat all levels, addressing surface texture, depth, and underlying tissue simultaneously. - Stronger collagen regeneration
Layering different modalities amplifies collagen production and promotes more thorough tissue remodelling, resulting in smoother and more resilient skin. - Fewer treatment sessions
By combining techniques, patients can achieve better results in a shorter overall timeframe, reducing the number of clinic visits without compromising outcomes.
This holistic, multi-modal approach is rapidly becoming the gold standard in scar treatment, offering patients more predictable, natural-looking results than single-modality therapies alone.
What Results Can You Expect in 2026?
With the new technologies coming next year, you can expect more predictable, more natural and more noticeable improvement. Scars that were previously resistant to treatment are now responding better because modern devices reach deeper layers without causing excess trauma.
You may notice smoother texture, improved skin tone, reduced depth of indentations and better blending with surrounding skin. Results develop over months rather than days because they rely on collagen regeneration rather than surface change alone.
FAQs:
1. What makes the new scar treatment technologies expected in 2026 different from current treatments?
The technologies arriving in 2026 are different because they focus more on regeneration and personalised tissue remodelling instead of simply resurfacing the skin. Older methods, like basic ablative lasers, tended to treat the top layer and relied on controlled injury to encourage healing. The newest innovations combine advanced imaging, adaptive energy delivery, biological signalling molecules and multi‑modal platforms that work at deeper levels of the skin. By encouraging the skin’s own repair mechanisms and tailoring energy delivery in real time, these treatments aim to improve collagen architecture, reduce abnormal scar tissue and deliver more natural‑looking, long‑lasting results with less trauma.
2. How do next‑generation fractional lasers improve scar treatment outcomes?
Next‑generation fractional lasers improve outcomes because they use real‑time feedback and adaptive energy control to map the unique depth and density of each scar during the treatment itself. Unlike older lasers that delivered uniform pulses regardless of tissue variation, the new systems adjust power, wavelength and penetration depth according to how the scar responds in real time. This helps treat both superficial irregularities and deeper scar components within the same session. The result is a more targeted remodelling process that can reduce downtime, improve texture and encourage more organised collagen regeneration, which leads to smoother skin.
3. Why are topical biologics considered a major innovation for scar prevention and early treatment?
Topical biologics represent a major innovation because they do more than reduce visible scarring; they interact at a cellular level to influence how scars form in the first place. These products contain molecules such as peptides, growth factors and exosome‑derived signals that communicate with fibroblasts, the cells responsible for collagen production. By guiding these cells toward a more organised, regulated healing response, biologics can reduce excessive collagen build‑up, prevent abnormal tissue formation and help minimise pigmentation changes early in the healing process. This shift toward prevention rather than repair is one of the most exciting aspects of 2026 scar care.
4. How have enhancements in RF microneedling increased its effectiveness for scars?
Enhancements in radiofrequency microneedling increase effectiveness because the new devices deliver heat more uniformly and penetrate scar tissue more deeply with better precision. Previously, RF microneedling treatments could sometimes be uneven or limited in depth, which constrained how well the thermal stimulation remodelled deeper layers. The upgraded platforms dynamically adjust needle depth and energy intensity across varying scar thicknesses, targeting both shallow and deep scar components within a single session. This leads to more consistent collagen remodelling, improved texture, and higher patient satisfaction, especially for mixed and tethered scars.
5. In what ways do injectable regenerative therapies differ from traditional dermal fillers?
Injectable regenerative therapies differ from traditional dermal fillers because they are designed not simply to add temporary volume, but to encourage long‑term tissue improvement. Traditional fillers typically provide immediate volume beneath an indentation, which can improve appearance for a time but does not change the underlying scar structure. Regenerative injectables contain substances that activate collagen production and improve the extracellular matrix, leading to real tissue remodelling over months and years. These therapies can soften depressed scars, improve firmness and enhance the skin’s quality in a way that continues to evolve long after treatment.
6. What advantages do hybrid laser‑RF devices offer over single‑modality treatments?
Hybrid laser‑RF devices offer advantages because they combine two different forms of energy to address multiple aspects of a scar in one system. Fractional lasers are excellent at resurfacing and encouraging organised outer tissue regeneration, while RF microneedling stimulates deep collagen remodelling through controlled thermal stimulation. When these energies are used in a coordinated way, dermatologists can treat surface texture, mid‑dermal abnormalities and deeper fibrotic structures concurrently. This multi‑layer approach often results in faster improvement, fewer total sessions, and a more comprehensive correction than treatments that focus on one layer at a time.
7. Can the new light therapies (like collagen‑modulating LLLT) replace other aggressive treatments?
While collagen‑modulating light therapies, including advanced low‑level light therapy (LLLT) and specialised LED systems, offer gentle improvement, they are not typically a full replacement for more aggressive treatments. These advanced light systems work by influencing cellular metabolism, reducing inflammation and supporting better collagen organisation. They are especially useful as supportive or follow‑up treatments after stronger interventions like lasers or microneedling, helping maintain improvement and regulate pigmentation. For highly irregular or severe scars, more substantial remodeling tools remain essential, but light therapy plays a valuable role in a combined strategy.
8. Are there specific scars that benefit more from certain innovative treatments?
Yes, certain scars respond better to specific innovations because different scars involve distinct structural and biological characteristics. For example, indented acne scars often benefit most from enhanced RF microneedling, hybrid devices and regenerative injectables because these modalities stimulate deep collagen production and lift depressed areas. Raised surgical scars, which may involve excess fibrotic tissue, often respond well to biologics that regulate collagen synthesis, fractional lasers that improve texture, and ultrasound tightening that softens rigid tissue. Fresh wounds at high risk of scarring may benefit most from early biologic intervention, which can guide healing and reduce long‑term hyperplasia.
9. What should patients realistically expect in terms of results and timelines with the 2026 treatments?
Patients should expect that results from the newest scar treatments will generally appear gradually over several months rather than instantly, because many of these innovations work by stimulating biological regeneration. Unlike simple resurfacing that may show improvement within days, approaches that remodel collagen, improve extracellular matrix quality or influence fibroblast activity depend on the body’s healing cycles. Over time, patients often see smoother texture, improved skin tone, reduced depth of indentations and a more natural blending with surrounding skin. The most dramatic improvements typically take place over three to six months, with continued refinement up to a year after treatment.
10. How do combination therapy plans improve scar treatment outcomes in 2026?
Combination therapy plans improve outcomes because they allow dermatologists to address multiple layers and mechanisms of scarring simultaneously. Scar tissue is complex, involving changes at the surface, within the dermis and at deeper structural levels. By carefully sequencing technologies for instance, starting with biologics to condition the tissue, followed by hybrid laser‑RF treatments to remodel architecture, and finishing with light therapy to support regeneration clinicians can achieve more thorough improvement than any single modality alone. This layered approach often reduces the total number of treatments needed, enhances predictability, and delivers a more balanced, natural‑looking result.
Final Thought: The Future of Scar Treatment
The year 2026 is set to redefine how we approach scar management, offering solutions that are more precise, regenerative, and tailored than ever before. From next-generation fractional lasers and biologics to hybrid devices and advanced RF microneedling, the innovations discussed promise improved outcomes for a wide range of scars. For patients, this means not only smoother, more natural-looking skin but also shorter recovery times and treatments designed to work with the body’s own healing processes.
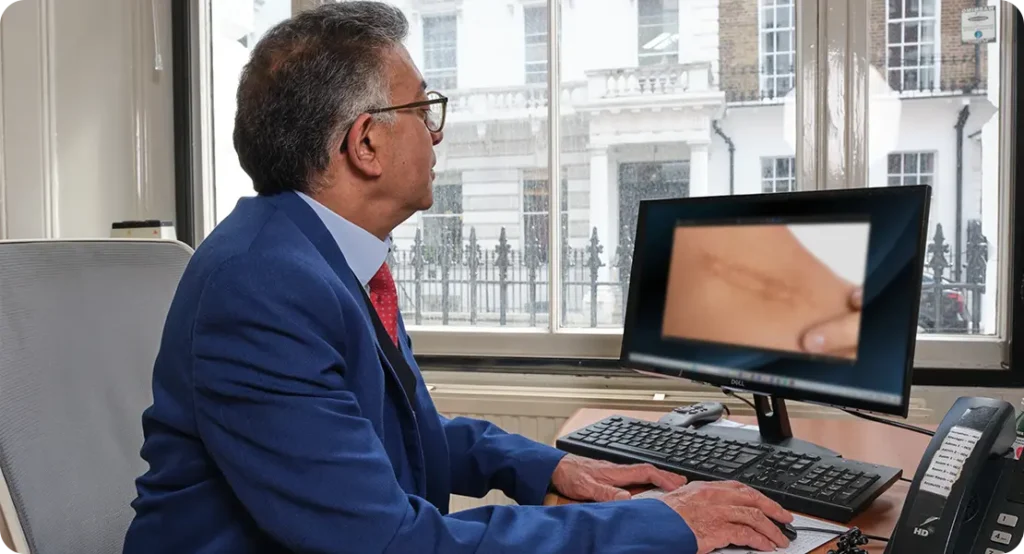
If you’re considering scar treatment in London, you can contact us at London Dermatology Centre to book a consultation with one of our specialists and discuss which combination of therapies is best suited to your needs.
References:
1. Ptaszek, B. (2025) ‘The use of a fractional CO₂ laser in acne scar treatment a systematic review’, Life, 15(6), p. 915. https://www.mdpi.com/2075-1729/15/6/915
2. Măgerușan, Ș.E. (2024) ‘Current understanding of microneedling procedures for acne skin: a narrative review’, Cosmetics, 11(6), p.193. https://www.mdpi.com/2079-9284/11/6/193
3. Niaz, G. et al. (2025) ‘A systematic review of current evidence on fractional radiofrequency microneedling for acne scarring’, Journal of Dermatologic Surgery and Research, [online]. https://pubmed.ncbi.nlm.nih.gov/39781098/
4. Meghe, S. et al. (2024) ‘Efficacy of microneedling and CO₂ laser therapy for acne scar remodelling: a comprehensive review’, Cureus, 16(2), e55092. https://pubmed.ncbi.nlm.nih.gov/38558661/ 5. Zhang, M. et al. (2025) ‘Advances in the treatment of acne scars’, Journal of Plastic, Reconstructive & Aesthetic Surgery [online]. https://pmc.ncbi.nlm.nih.gov/articles/PMC12425707/
