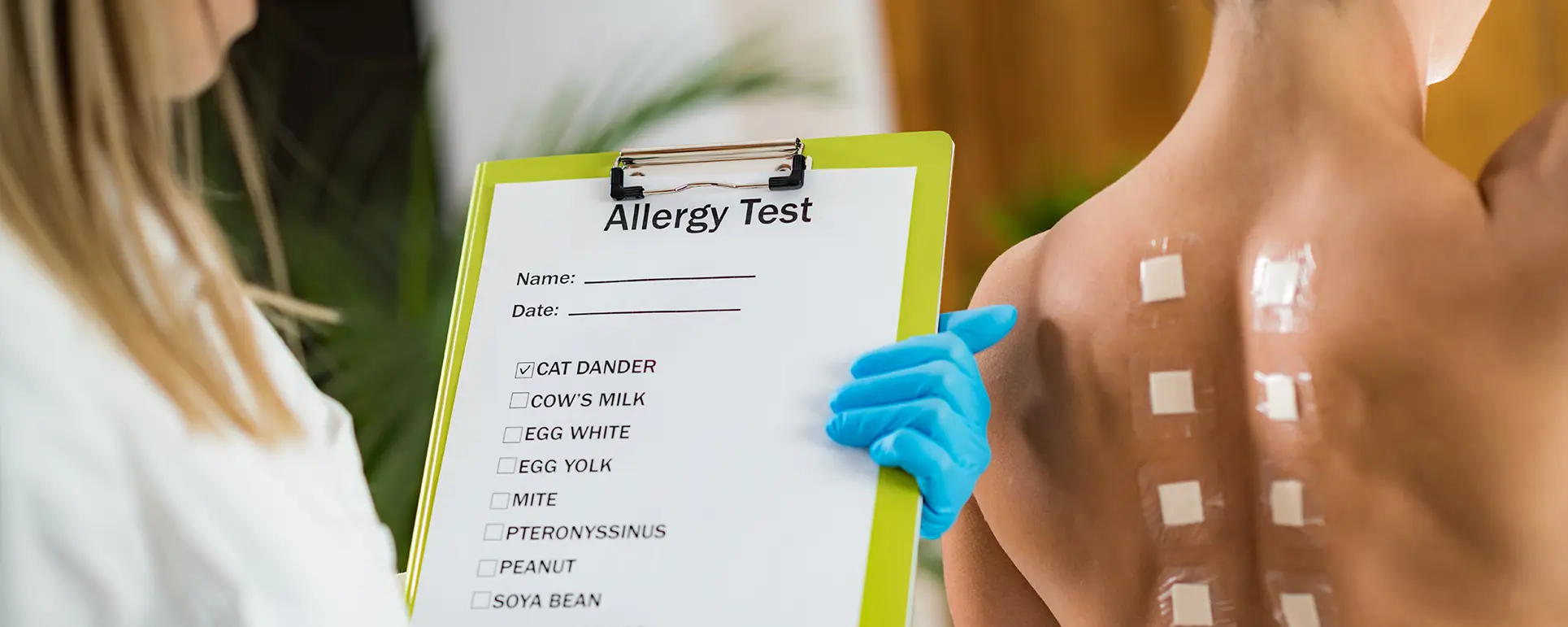
Patch testing has long been the cornerstone of diagnosing allergic contact dermatitis (ACD), a condition triggered by direct skin exposure to allergens. Despite its effectiveness, the traditional method has limitations, often depending heavily on the skill of the clinician and the subjective interpretation of results.
In recent years, scientific advancements and technological integration have led to notable changes in how patch tests are conducted, read, and interpreted. These improvements are not only increasing diagnostic accuracy but also making the process more efficient and accessible to patients.
From broader allergen panels informed by population studies to artificial intelligence (AI)-driven image analysis, patch testing is becoming more tailored and responsive to the individual needs of each patient.
These advancements represent a shift towards precision dermatology, where diagnostics are underpinned by robust data and supported by digital tools, ensuring clinicians can deliver faster, more reliable outcomes.
A New Era in Allergy Diagnosis
The classical model of patch testing involves the application of potential allergens on the skin, typically the back, and evaluating skin responses over a series of days. While the process is effective in many cases, it is inherently subjective, relying on visual assessment and clinician experience to score skin reactions such as erythema, oedema, or vesiculation.
The new wave of research-driven protocols aims to reduce this subjectivity. Digital photography, combined with standardised scoring algorithms, is enabling more accurate and reproducible results. Furthermore, these tools allow for the comparison of skin responses over time with a level of detail previously unattainable in traditional methods.
Innovations in image recognition software are making it possible to automate the detection of subtle skin changes, minimising observer bias and improving diagnostic confidence. These changes are especially valuable in complex cases where minor differences in skin response can affect the clinical outcome. In short, technology is shifting patch testing from an art to a science.
Expanding Allergen Panels Based on Population Data
Historically, patch testing was limited to a narrow selection of common allergens such as nickel, fragrances, and preservatives. This limited scope sometimes resulted in inconclusive diagnoses, especially as exposure to new chemicals in modern environments has grown. In response, allergen panels are now being expanded based on rigorous epidemiological research and national surveillance data.
Dermatology societies across Europe and North America are updating standard series to reflect the allergens most relevant to current populations, including substances found in electronics, cosmetics, adhesives, and new occupational materials. This evidence-led approach ensures that clinicians are not only testing for the most likely culprits but are also capturing emerging allergens that may otherwise go unnoticed.
Additionally, tailored series are now available for specific industries, age groups, and geographical locations, offering a more customised diagnostic process. The result is a significantly higher detection rate of clinically relevant allergens, allowing for more effective patient education and targeted avoidance strategies.
Digital Patch Readers: Precision Through Technology
One of the most transformative innovations in patch testing is the development of digital patch readers. These devices utilise high-resolution cameras and AI-driven software to scan and analyse skin test areas, providing objective measurements of reaction severity. Unlike manual assessments, which can vary depending on clinician interpretation and lighting conditions, digital readers offer consistent, quantifiable results.
This has significantly improved inter-rater reliability and has reduced diagnostic errors due to misinterpretation or oversight. Some systems are also capable of storing images over time, enabling longitudinal comparisons that help identify delayed reactions or evolving sensitivity patterns. The integration of these tools into routine practice represents a major leap forward in the standardisation of patch testing.
Furthermore, digital readers are proving especially valuable in research settings, where consistency and reproducibility are paramount. By offering an unbiased assessment of skin reactions, these devices are helping to set new benchmarks for diagnostic accuracy in dermatology.
Evidence-Based Scoring and Standardisation
In tandem with technological advancements, there has been a concerted effort to standardise the scoring of patch test reactions. Historically, clinicians used varied methods and criteria to grade the severity of reactions, which often led to discrepancies in diagnosis and management.
Today, dermatological societies such as the European Society of Contact Dermatitis (ESCD) have developed and promoted standardised scoring guidelines that define specific reaction parameters—such as erythema intensity, papule presence, and vesicle formation—with clear, reproducible criteria.
This not only ensures consistency across clinical settings but also facilitates better communication and comparison of data across international studies. Additionally, training programmes now incorporate these standards into clinician education, enhancing diagnostic skills from the outset.
These structured systems are particularly beneficial for multidisciplinary teams, where shared language and expectations improve collaboration. Ultimately, standardised scoring frameworks are making patch testing more transparent and replicable, aligning it with broader trends in evidence-based medical practice.
Incorporating Non-Invasive Biomarkers
Recent research has begun exploring how biomarkers can enhance the diagnostic power of patch testing. By analysing immune responses at the molecular level, dermatologists can now gain insights into the skin’s reactivity beyond visible symptoms. Techniques such as tape stripping allow clinicians to collect skin surface samples for cytokine and chemokine analysis, providing a biochemical snapshot of inflammatory processes.
These biomarkers can help differentiate between irritant and allergic reactions, which often appear similar but require different management strategies. Moreover, early findings suggest that certain biomarkers may predict delayed or subclinical reactions, offering a window into allergic sensitivity even before full clinical symptoms manifest.
This could be particularly useful in patients with a history of atypical or intermittent dermatitis. While biomarker testing is still in development and not yet widely used in clinical practice, its integration into patch testing protocols holds great promise. It adds a valuable layer of precision, making diagnoses more nuanced and potentially more predictive of long-term outcomes.
At-Home Patch Testing: A Controversial but Growing Trend
As telemedicine becomes increasingly prevalent, the concept of at-home patch testing has emerged as a potential solution for patients in remote or underserved areas. These kits are designed for patient use under virtual supervision from a dermatologist and include detailed instructions for application, monitoring, and reporting.
Early pilot programmes have shown mixed results: while convenient, the success of at-home testing relies heavily on patient compliance, understanding, and proper image submission. Concerns about improper placement, reaction misinterpretation, or poor photographic quality persist. However, when supported by strong digital platforms and clear communication protocols, at-home patch testing may serve as a useful adjunct to traditional methods, especially for initial screening or follow-up testing.
Further research is needed to validate its reliability and safety on a larger scale. If refined and standardised, at-home testing could reduce diagnostic delays, improve access to care, and offer a more flexible approach to allergy management for suitable patient populations.
Artificial Intelligence and Machine Learning Applications
Artificial intelligence (AI) and machine learning (ML) are beginning to revolutionise how patch test data is interpreted. These technologies are being trained on vast datasets of clinical images and patient outcomes to recognise patterns, grade reaction severity, and even suggest likely allergens based on patient history.
This level of computational analysis provides an extra layer of decision support for dermatologists, particularly in complex cases involving multiple or borderline reactions. AI algorithms can also help identify rare or under-reported allergens that may otherwise be overlooked. In the future, machine learning may enable predictive diagnostics, helping clinicians assess the likelihood of sensitisation before a patient even undergoes a test. Such tools are especially valuable in occupational dermatology, where exposure risk can be high and early intervention is critical.
While still in its infancy, AI’s role in patch testing is rapidly expanding, and it promises to augment—not replace—clinical expertise with data-driven insights that enhance both accuracy and efficiency.
Real-Time Monitoring and Mobile Apps
Modern dermatology is embracing real-time monitoring tools to capture reactions that occur outside the clinic. Mobile apps designed for patch testing allow patients to log their symptoms and upload photos at specified intervals during the testing period. These tools bridge the gap between in-clinic assessments and the delayed nature of some allergic reactions.
Dermatologists can access these uploads instantly, offering feedback or revising initial assessments if necessary. Additionally, time-stamped photo records can be archived for long-term comparison or research use. This system not only increases diagnostic accuracy but also empowers patients to take an active role in their care. As mobile health tools become more sophisticated, features like automated reaction detection, symptom tracking, and patient reminders are being integrated into these apps.
Real-time monitoring is proving particularly valuable in managing delayed hypersensitivity reactions, which may peak days after allergen application. By extending clinical oversight beyond the appointment, mobile apps are significantly enriching the patch testing experience.
Training and Competency Standards in Modern Patch Testing
With the influx of new tools, scoring systems, and digital diagnostics, proper clinician training has never been more crucial. Dermatology associations are now placing strong emphasis on continuous education, ensuring clinicians remain competent in both traditional patch test interpretation and emerging digital systems.
Training curricula include modules on the use of digital patch readers, AI-assisted tools, and interpreting biomarker data. In clinical practice, experienced consultants often mentor newer staff, reinforcing standardisation and best practices.
Conferences and workshops are increasingly focused on hands-on digital demonstrations and case study analysis, which help bridge the gap between theory and practice. Maintaining a high level of competency ensures not only accurate diagnostics but also consistent patient outcomes across different healthcare providers.
As patch testing grows more nuanced and technologically enhanced, ongoing professional development becomes essential for dermatologists, nurses, and research teams alike. High-quality training is a cornerstone of patient safety and diagnostic integrity in this rapidly evolving field.
Addressing False Negatives and Cross-Reactivity
False negatives remain a challenge in patch testing, especially in patients with low-grade or infrequent exposures. These can lead to misdiagnosis or continued contact with the offending allergen. Researchers have discovered that repeated open application testing (ROAT) or testing with higher concentrations—within safe limits—can sometimes unmask elusive allergens.
Furthermore, the introduction of cross-reactivity maps based on molecular similarity between compounds allows dermatologists to consider related allergens that might provoke a reaction despite not being directly tested. This is particularly important in patients with occupational exposure to complex chemical families or multiple skincare products. For example, a patient reacting to one type of fragrance may also show sensitivity to structurally similar compounds found in unrelated items.

Addressing cross-reactivity is a matter of expanding clinician awareness and refining test panels accordingly. By improving allergen coverage and diagnostic methodology, the risk of false negatives is reduced, ensuring patients receive the correct diagnosis and avoid prolonged suffering or unnecessary treatment.
Integrating Patch Testing into Broader Dermatological Care Pathways
As dermatology moves towards more holistic, integrated care models, patch testing is increasingly being positioned within wider diagnostic and treatment pathways. For patients presenting with chronic eczema, unexplained rashes, or suspected allergic contact dermatitis, patch testing can serve as a pivotal first step that informs downstream decisions.
When test results are synchronised with clinical history, lifestyle evaluation, and other diagnostic tools like skin biopsies or phototesting, they offer a clearer, multi-dimensional understanding of the patient’s condition. In multidisciplinary settings—such as allergy clinics, occupational health departments, and immunology units—patch testing contributes to collaborative care planning, ensuring interventions are aligned and comprehensive.
This integrative approach helps reduce the recurrence of dermatitis by targeting both the root cause and any contributing environmental factors. Embedding patch testing into a coordinated care framework not only improves diagnostic efficiency but also enhances long-term patient outcomes by ensuring consistent follow-up, tailored education, and ongoing prevention strategies.
Psychological Impact and the Value of Clear Diagnosis
For many patients, the impact of undiagnosed or poorly managed allergic contact dermatitis goes beyond the skin. Persistent symptoms such as itching, visible rashes, and discomfort can lead to psychological distress, social embarrassment, and even reduced work productivity. In this context, the value of an accurate patch test diagnosis cannot be overstated.
Receiving a definitive answer empowers patients to take control of their condition through allergen avoidance and informed lifestyle adjustments. Clinicians also play a critical role in educating patients on their results, helping them navigate ingredient labels, occupational risks, and product choices. Digital resources and post-diagnostic counselling sessions are increasingly being used to support this educational effort.

As a result, patients often report a sense of relief and improved mental well-being after understanding the cause of their symptoms. A clear diagnosis can turn months—or years—of frustration into actionable steps toward recovery, underscoring the psychological and emotional benefits of modern patch testing.
Emerging Allergen Sources: Textiles, Electronics, and Nanomaterials
The expanding scope of patch testing is increasingly driven by emerging sources of allergens found in everyday products. Advances in wearable technology, for example, have introduced new materials such as nickel alloys, rubber adhesives, and conductive fabrics that can trigger contact dermatitis in sensitive individuals. Similarly, nanomaterials—used in cosmetics, sunscreens, and clothing—pose new challenges due to their small particle size and potential for skin penetration.
Textile dyes and finishes, often overlooked, are now recognised as common culprits, particularly in patients experiencing localised reactions on pressure points or seams. Research is focusing on identifying and standardising these newer allergen sources, allowing them to be incorporated into extended patch test panels.
This expansion is critical as patients increasingly present with dermatitis linked to lifestyle innovations and modern consumer goods. Staying ahead of these emerging exposures ensures patch testing remains clinically relevant and responsive to evolving patterns of sensitisation in the general population.
Policy and Regulatory Implications of Patch Test Research
The growing body of research surrounding patch testing also has implications for public health policy and product regulation. As more allergens are identified and validated through epidemiological studies, regulatory bodies may introduce labelling requirements or restrict the use of high-risk substances in consumer products.
For instance, the European Union’s Cosmetic Products Regulation already mandates disclosure of certain allergens, a move supported by patch test data showing rising sensitivity rates. Dermatologists and researchers play a key role in these regulatory processes by submitting surveillance data, participating in safety reviews, and publishing findings that inform policy decisions.
Moreover, patch testing can highlight occupational risks that warrant regulatory oversight, particularly in industries involving chemical processing, construction, or healthcare. By bridging clinical practice and public policy, patch test research not only benefits individual patients but also contributes to broader efforts in allergen risk reduction, consumer safety, and workplace health protection.
Final Thoughts: Making Patch Testing Smarter and More Accessible
Patch testing is entering a new phase—one defined by precision, objectivity, and accessibility. Technological advances such as AI, digital patch readers, and real-time monitoring are eliminating many of the shortcomings that have historically limited diagnostic accuracy.
Meanwhile, expanded allergen panels and standardised scoring systems are ensuring broader coverage and more reliable interpretation. Together, these innovations are making patch testing not only smarter but also more patient-centric. In an era where personalisation is the gold standard of care, dermatologists now have more tools than ever to tailor their diagnostic process to each individual.
Looking ahead, as digital platforms, biomarker insights, and machine learning become more integrated into dermatological practice, patch testing will likely continue to evolve into an even more precise and effective diagnostic technique.
If you would like to have an allergy test done, you can contact us at The London Dermatology Centre for a consultation with one of our experienced dermatologists.
References
- Johansen, J.D., Aalto-Korte, K., Agner, T., Andersen, K.E., Bircher, A., Bruze, M., Cannavó, A., Giménez-Arnau, A.M., Gonçalo, M., Goossens, A. and Lepoittevin, J.P., 2015. European Society of Contact Dermatitis guideline for diagnostic patch testing – recommendations on best practice. Contact Dermatitis, 73(4), pp.195–221.
– A comprehensive guideline widely referenced in clinical practice for optimising patch testing protocols across Europe. - Duarte, I., Silvestre, J.F., Ayala, F., Diepgen, T.L., Hughes, T.M. and Svedman, C., 2022. Patch testing today: Practical challenges and future perspectives. Journal of the European Academy of Dermatology and Venereology, 36(8), pp.1207–1214.
– Discusses current limitations in patch testing and research-led solutions improving diagnostic accuracy. - Warshaw, E.M., Belsito, D.V., Taylor, J.S., Maibach, H.I., Fowler, J.F., DeKoven, J.G., Sasseville, D., Pratt, M.D. and Zug, K.A., 2017. North American Contact Dermatitis Group patch test results: 2015–2016. Dermatitis, 28(1), pp.33–46.
Available at: https://journals.lww.com/dermatitis/Fulltext/2017/28010/North_American_Contact_Dermatitis_Group_Patch.5.aspx [Accessed 13 May 2025].
– A valuable data set highlighting trends in allergen positivity rates and interpretation in North American populations. - National Institute for Health and Care Excellence (NICE), 2021. Contact dermatitis: Assessment and management. London: NICE.
Available at: https://www.nice.org.uk/guidance [Accessed 13 May 2025].
– Official UK guidance on the assessment and referral pathways for suspected allergic contact dermatitis, including when patch testing is appropriate. - Lachapelle, J.M., 2012. A proposed relevance scale for the interpretation of contact allergy. Contact Dermatitis, 67(4), pp.193–196.
– Presents a clinically useful model for interpreting the real-world significance of positive patch test results in individual patients.