Contact dermatitis is a skin condition that results from direct contact with a substance that irritates the skin or triggers an allergic reaction. It’s one of the most common reasons people visit a dermatologist, particularly when the rash becomes persistent, uncomfortable, or difficult to identify. The process of diagnosing and treating contact dermatitis involves a detailed assessment, tailored management, and preventative strategies designed to keep flare-ups under control.
How Diagnosis Begins
When the rash appeared and how it has changed
Dermatologists begin by asking when the skin problem first started and how it has progressed over time. The timeline of symptoms often offers essential clues—an immediate reaction may point towards an irritant, whereas a delayed onset might suggest an allergic response. They’ll also want to know whether the rash appeared suddenly, spread to new areas, or improved with any self-care measures.
They’ll also ask about any patterns in the rash. For example, if the symptoms come and go or appear after specific activities, that could indicate a recurring exposure to a trigger. Tracking the evolution of the rash helps rule out other conditions such as eczema or fungal infections, which may look similar but behave quite differently.
Where on the body it occurs
The location of the rash can help narrow down the possible causes. Contact dermatitis often appears in areas that come into frequent contact with specific substances—hands, wrists, face, neck, and eyelids are common trouble spots. If the rash appears symmetrically on both hands, it might be linked to something like soap or sanitiser, while a patch on one wrist could point to a watch strap or bracelet.
Dermatologists also consider whether clothing, personal care items, or even work equipment could be responsible. For example, a rash around the waistband might indicate a reaction to metal fasteners, while an outbreak on the cheeks could be due to cosmetic products or a mobile phone case. Every bit of location-specific detail matters when narrowing down the list of culprits.

Products recently used (skincare, detergents, cosmetics)
Information about recent product use is another vital part of the diagnostic process. Dermatologists will ask about any new soaps, moisturisers, perfumes, or makeup products. Even “natural” or “organic” items can contain allergens like essential oils, so it’s important not to rule anything out prematurely. They’ll also look into what detergents are being used for laundry, as residue left on clothing can affect the skin.
Often, people don’t realise that even long-used products can suddenly trigger a reaction. This is because allergic contact dermatitis can develop over time, after repeated exposure to the same ingredient. Dermatologists usually ask patients to bring a list of their products—or the actual items themselves—so that ingredients can be reviewed in detail.
Work and hobbies that may involve irritants or allergens
Your job or hobbies might expose you to substances that can irritate your skin or trigger an allergic response. Hairdressers, healthcare workers, cleaners, and mechanics are particularly vulnerable due to frequent contact with chemicals, water, gloves, or powders. Dermatologists ask targeted questions about occupational tasks to identify potential problem exposures.
Hobbies can be just as revealing. Gardening may involve exposure to plant-based allergens, while painting or model-building can involve solvents, glues, or resins. If you’ve taken up something new recently—even something as seemingly harmless as DIY crafts—it can play a significant role in the development of symptoms.
Previous history of allergies or eczema
A history of other allergic conditions, like hay fever, asthma, or atopic eczema, can increase the likelihood of developing contact dermatitis. Dermatologists take this into account because individuals with sensitive or reactive skin are generally more prone to irritation and allergic responses.
In addition to personal history, they may ask whether close family members also have skin conditions or known sensitivities. While contact dermatitis itself isn’t inherited, certain skin types and immune tendencies can be, which may raise the risk of developing persistent or severe reactions to common substances.
Examination and Patch Testing
The shape and distribution of the rash
Dermatologists examine the edges, borders, and spread of the rash to assess whether it suggests contact with an external substance. A well-defined area might indicate a specific item—like a watch or adhesive bandage—while a more diffuse rash could be due to frequent exposure to water or airborne allergens. Sharp outlines often point to direct contact, whereas more widespread patterns suggest irritants like cleaning agents or personal care products.
They also look for subtle signs like skin thickening or cracking, which indicate chronic exposure or delayed treatment. In some cases, contact dermatitis overlaps with other skin conditions, so a detailed visual assessment helps rule out alternatives like psoriasis or fungal infections.
Whether the skin is dry, blistered, cracked, or inflamed
The physical condition of the affected skin reveals how severe or long-standing the problem is. Blistering often suggests a strong allergic response, especially if accompanied by intense itching. Dry, cracked, and scaly skin may reflect repeated irritation, which slowly breaks down the skin’s natural barrier. Dermatologists consider all these aspects when forming a diagnosis.
They also check for signs of secondary infection, which can occur if the skin is broken from scratching or long-term inflammation. If infection is suspected, swabs might be taken for testing. The state of the skin informs not just the diagnosis but also the intensity and type of treatment prescribed.
Patch testing
If an allergic cause is suspected, patch testing is often used. This involves applying small amounts of various potential allergens to the back under adhesive strips. The patches are usually left in place for 48 hours, then the skin is assessed again after 72 hours to identify any delayed allergic reactions.
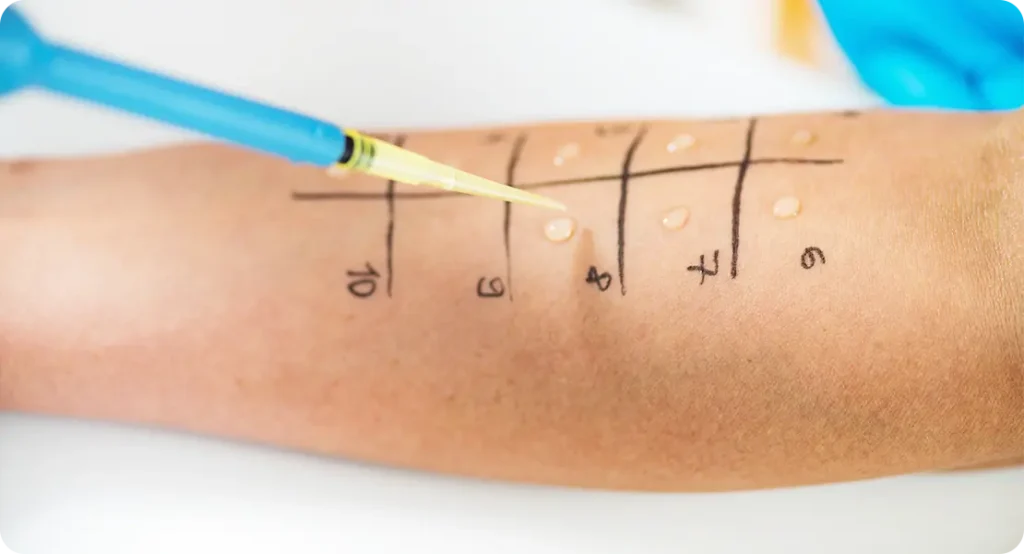
Patch testing is particularly helpful for confirming sensitivities to common allergens like preservatives, metals, or fragrances. Dermatologists use these results to give patients a clear list of substances to avoid. It’s a safe, controlled method that helps solve cases where the cause of the dermatitis isn’t immediately obvious.
Understanding the Two Types
Irritant Contact Dermatitis
This type occurs when a substance physically damages the skin’s outer layer. Common culprits include soaps, detergents, disinfectants, and solvents—especially when there’s frequent or prolonged contact. It’s often seen on the hands and forearms, particularly in people who wash their hands often or work in wet environments.
Unlike allergies, irritant contact dermatitis doesn’t involve the immune system. It can affect anyone if the exposure is strong enough or the skin is already compromised. People with naturally dry or sensitive skin are more susceptible, and once the skin barrier is damaged, it becomes more vulnerable to further irritation.
Allergic Contact Dermatitis
This is an immune reaction that happens when the body identifies a substance as a threat. The first exposure may not trigger any symptoms, but once the immune system becomes sensitised, future contact with even a small amount can cause a rash. Common allergens include nickel, fragrances, rubber additives, and certain preservatives.
The reaction usually appears one to three days after contact, often with redness, swelling, itching, and small blisters. Unlike irritant dermatitis, allergic contact dermatitis tends to recur in the same areas and won’t improve unless the allergen is completely avoided. It may also spread to areas not in direct contact, due to immune system involvement.
Immediate Treatment Approaches
Topical corticosteroids
These are anti-inflammatory creams or ointments prescribed to reduce redness, swelling, and itching. Dermatologists choose the strength of the steroid based on the location and severity of the rash. Mild cases might be treated with over-the-counter creams, while more serious flare-ups may require prescription-strength formulations.
Corticosteroids are typically used for a short course to avoid long-term side effects like skin thinning. Dermatologists usually advise applying the cream once or twice a day in a thin layer and may recommend tapering off use as symptoms improve. In sensitive areas like the face or groin, milder steroids are used with extra caution.
Oral corticosteroids
For widespread or severe flare-ups, short courses of oral steroids may be prescribed. These work throughout the body to quickly reduce inflammation and control the immune response. They’re particularly useful when rashes cover large areas or cause significant discomfort.
Because of their potential side effects, oral steroids are only used under close supervision. Dermatologists ensure the dosage and duration are carefully managed, and they’ll provide guidance on how to taper off the medication to avoid rebound symptoms.
Antihistamines
Oral antihistamines are sometimes used to control itching, particularly when it interferes with sleep or daily activities. They’re more effective for allergic contact dermatitis than for irritant types, but they can still help reduce the urge to scratch and allow the skin to heal.
Some antihistamines cause drowsiness and are best taken at night, while non-drowsy options can be used during the day. Dermatologists will usually tailor recommendations based on the patient’s lifestyle and symptoms.

Emollients
Moisturisers play a crucial role in restoring the skin’s natural barrier. Emollients help lock in moisture, soothe dryness, and protect the skin from further damage. Dermatologists often recommend fragrance-free, hypoallergenic formulations and may advise using them several times a day, especially after washing hands.
Regular use of emollients not only helps manage current flare-ups but also prevents future ones. When the skin is well hydrated and supported, it’s more resilient to both irritants and allergens.
Certainly — here’s the continuation and completion of the article, following the same structure and tone, with two original paragraphs per bullet point and no duplication from any online content.
Avoiding Future Flare-Ups
Switch to fragrance-free, hypoallergenic products
Fragrances are among the most common allergens in personal care products. Even products labelled “natural” or “for sensitive skin” can contain essential oils or plant extracts that trigger reactions. Dermatologists often advise switching to fully fragrance-free and hypoallergenic options, particularly for moisturisers, shampoos, soaps, and laundry detergents.
Using simple, non-irritating formulas helps avoid unnecessary exposure to potential allergens. Over time, reducing contact with problem ingredients gives the skin a chance to heal and become more resilient. Dermatologists may also provide a list of recommended products tailored to a patient’s known sensitivities.
Wear non-latex gloves for cleaning or wet work
Protecting your hands is crucial if you frequently come into contact with water or cleaning agents. Latex gloves can cause allergic reactions in some individuals, so non-latex alternatives such as nitrile gloves are often recommended. These provide a physical barrier without introducing another potential allergen.

It’s also important to use gloves correctly—this means wearing them for short periods and ensuring your hands are clean and dry before putting them on. Prolonged wear or sweaty conditions inside gloves can actually worsen dermatitis, so dermatologists may suggest cotton liners or regular breaks to let your skin breathe.
Apply barrier creams before exposure to irritants
Barrier creams form a protective film over the skin, helping to shield it from harsh substances. These are especially useful for people who can’t completely avoid irritants due to their job or daily routines. They work best when applied before exposure and alongside other protective measures like gloves or sleeves.
Dermatologists may recommend using barrier creams in workplaces where frequent handwashing, chemical exposure, or friction is unavoidable. When applied consistently, they can reduce the impact of irritants and help preserve the integrity of the skin barrier over time.
Avoid known allergens identified through patch testing
Once patch testing reveals a specific allergen, strict avoidance is essential to prevent future reactions. Dermatologists will often provide a written list of ingredients or materials to avoid and may even direct patients to databases or apps that help identify safe products.
Avoidance may require lifestyle adjustments, such as changing cosmetics, switching jewellery metals, or checking clothing labels for dyes and preservatives. The key is consistency—repeated exposure, even in small amounts, can trigger symptoms again and again, so vigilance is crucial for long-term control.
Use mild, non-soap cleansers for daily washing
Traditional soap can strip the skin of its natural oils, leaving it dry and more prone to irritation. Dermatologists typically recommend non-soap cleansers that are pH-balanced and free from common irritants like sodium lauryl sulphate. These cleansers are gentle on the skin while still effective at removing dirt and oil.
Incorporating a mild cleanser into your routine helps protect the skin barrier and prevent future flare-ups. It’s particularly important to use these after working with potential irritants, as harsh cleansers may worsen any minor damage that has already occurred. Regular use supports healing and helps maintain healthy skin.
Adjust work tasks or protective equipment
In occupational cases, dermatologists may suggest practical changes to reduce exposure to triggers. This could include rotating job duties, introducing more frequent breaks, or changing the type of tools and equipment used. Even small adjustments can make a significant difference in the skin’s condition over time.
Where avoidance isn’t possible, dermatologists may coordinate with occupational health services to recommend safer alternatives or improved protective measures. Employers often accommodate these changes once they understand the medical necessity, and this can lead to a healthier, more sustainable working environment.
Seek support from occupational health if needed
Some cases of contact dermatitis, particularly those related to work, may require formal involvement from occupational health services. Dermatologists may write reports outlining the diagnosis and offering guidance on workplace adjustments or protective protocols.
Occupational health teams can help enforce changes, provide alternative products, and monitor your progress over time. This collaborative approach ensures you’re not repeatedly exposed to harmful substances and that your work environment supports your recovery.
Follow up regularly to monitor skin condition
Dermatologists often recommend regular follow-up appointments to monitor your progress, especially in chronic or recurring cases. These check-ins help assess whether the current treatment plan is effective or needs to be adjusted. Skin can change over time, and what worked at the start may not always be suitable later on.
Ongoing support also gives you the chance to discuss new products, symptoms, or exposures that might arise. Contact dermatitis often requires a bit of trial and error, so having a dermatologist guide you through that process can make all the difference in staying comfortable and flare-free.
Final Thoughts
Contact dermatitis may be common, but that doesn’t make it any less disruptive. Getting the right diagnosis from a dermatologist is the first and most important step. With a clear understanding of whether your reaction is irritant or allergic, you can begin treatment that actually works and, more importantly, make changes that stop the problem from coming back.
If you’re concerned about contact dermatitis, you can contact us at The London Dermatology Centre to arrange a consultation with one of our expert private dermatologists.
Managing contact dermatitis successfully comes down to three core principles: recognising the cause, treating the symptoms, and avoiding future triggers. Once these are in place, most people find that their skin becomes far more stable and comfortable. It takes a bit of patience and care, but with the right guidance, clear skin is well within reach.
