Dermatopathologists are a vital link between dermatology and pathology, offering in-depth insights into skin diseases that help guide diagnosis and treatment. Despite their importance, many patients are unsure about what dermatopathologists actually do and when they might become involved in their care. Below, we’ve answered 19 of the most frequently asked questions about dermatopathologists to help shed some light on this often-overlooked speciality.
1. What is a dermatopathologist?
A dermatopathologist is a medical doctor who specialises in diagnosing skin disorders by examining tissue samples under a microscope. They are highly trained in both dermatology and pathology, making them uniquely equipped to identify various skin diseases at a cellular level. This expertise allows them to provide crucial diagnostic support to dermatologists and other clinicians.
These specialists are particularly skilled in recognising subtle differences in skin biopsies that might be missed by general pathologists. From inflammatory skin conditions like psoriasis and eczema to complex skin cancers like melanoma, dermatopathologists can provide accurate diagnoses that directly influence treatment plans.
In clinical practice, a dermatologist often performs a skin biopsy and sends the sample to a dermatopathologist for evaluation. The dermatopathologist then issues a detailed report outlining the diagnosis, sometimes even suggesting additional tests if needed. Their findings play a major role in guiding both immediate and long-term patient management.
2. How is a dermatopathologist different from a dermatologist?
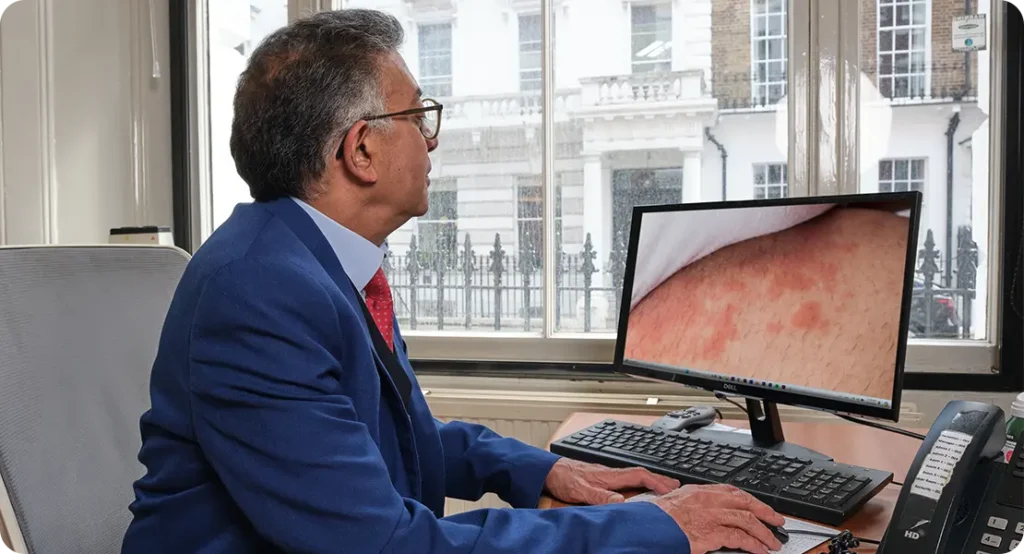
While both dermatologists and dermatopathologists deal with skin diseases, their roles are quite distinct. A dermatologist works directly with patients, diagnosing and treating skin conditions through physical exams, procedures, and prescriptions. In contrast, a dermatopathologist typically works behind the scenes, analysing skin tissue samples in a lab setting to provide a precise diagnosis.

Dermatopathologists do not usually see patients face-to-face. Instead, they receive biopsy samples taken by dermatologists or surgeons, and their work focuses on interpreting those samples. Their expertise lies in understanding skin pathology at a microscopic level, which allows them to identify diseases that are difficult to diagnose through visual inspection alone.
The two roles complement each other. A dermatologist may suspect a condition based on what they see and feel during a consultation, but confirmation often requires microscopic analysis. That’s where the dermatopathologist steps in, acting as a diagnostic detective whose findings help guide further clinical decisions.
3. When might I need to see a dermatopathologist?
Most patients don’t directly see a dermatopathologist, as their involvement is usually behind the scenes. However, if you’ve had a skin biopsy done, there’s a good chance a dermatopathologist has reviewed your sample. Their role is essential when a precise diagnosis is needed to determine the next steps in treatment.
You might indirectly be under the care of a dermatopathologist if your dermatologist encounters an unusual rash, a suspicious mole, or a persistent skin lesion that doesn’t respond to treatment. These cases often require a biopsy, which is then sent for detailed analysis to determine the exact nature of the condition.
While you may never meet a dermatopathologist in person, their report can significantly impact your diagnosis and treatment plan. Some complex or rare skin diseases can only be accurately diagnosed through histological analysis, making the dermatopathologist’s input vital to your care.
4. What kind of training does a dermatopathologist have?
Dermatopathologists undergo extensive training. After completing medical school, they typically specialise in either dermatology or pathology during their residency. Following that, they pursue a fellowship in dermatopathology, which involves in-depth training in both skin disease and microscopic interpretation of skin samples.
This dual training ensures that dermatopathologists are well-versed in both clinical dermatology and laboratory-based pathology. Their education enables them to bridge the gap between what is observed on the skin’s surface and what is occurring at a cellular level. It’s this unique combination that sets them apart from general pathologists or dermatologists working alone.
In addition to clinical training, dermatopathologists are often involved in research and continuous education. They keep up to date with advances in immunohistochemistry, molecular diagnostics, and other emerging technologies that aid in accurate and early diagnosis of skin diseases.
5. What types of conditions do dermatopathologists diagnose?
Dermatopathologists diagnose a wide range of conditions, from common inflammatory skin diseases to rare and aggressive cancers. They play a crucial role in identifying skin cancers such as basal cell carcinoma, squamous cell carcinoma, and melanoma. Early and accurate identification of these cancers can significantly impact patient outcomes.
Apart from cancer, dermatopathologists also help diagnose inflammatory conditions like lupus, lichen planus, and eczema. Many of these diseases can look similar on the surface but have distinctive microscopic features. Their detailed analysis ensures that patients receive the correct diagnosis and, subsequently, the most effective treatment.
They also play a role in diagnosing infectious diseases of the skin, autoimmune disorders, and blistering conditions. Because these diseases often present with overlapping clinical signs, microscopic examination by a dermatopathologist is key to unravelling their true nature.
6. How long does it take to get results from a dermatopathologist?
The turnaround time for a dermatopathology report can vary, but most results are available within one to two weeks. In urgent cases, preliminary results may be available sooner, particularly if a malignancy is suspected. The exact timing depends on the complexity of the sample and whether additional tests are required.

Some biopsies are straightforward and can be diagnosed quickly, while others require more time due to the need for special stains, deeper sections, or expert consultations. These additional steps are taken to ensure the highest level of diagnostic accuracy.
Patients are typically informed of their results by their dermatologist or GP, who receives the dermatopathologist’s report. If there are any unclear or unexpected findings, the dermatologist may discuss the results in more detail or recommend further testing.
7. Can dermatopathologists detect skin cancer?
Yes, detecting skin cancer is one of the primary responsibilities of a dermatopathologist. When a dermatologist removes a suspicious mole or lesion, the tissue is sent to a dermatopathologist for detailed examination. They look for abnormal cell structures and growth patterns that could indicate basal cell carcinoma, squamous cell carcinoma, or melanoma.
Their expertise is essential in determining whether a lesion is benign, precancerous, or malignant. In the case of melanoma, for example, the dermatopathologist assesses the depth of invasion, cellular atypia, and mitotic rate—factors that are crucial for staging and guiding treatment decisions.
Accurate cancer diagnosis depends heavily on the dermatopathologist’s findings. Their report not only confirms the presence of cancer but may also include recommendations for further treatment, such as re-excision or referral to oncology, making their role critical in the patient’s care pathway.
8. Do dermatopathologists work in hospitals or private labs?
Dermatopathologists can work in a variety of settings, including hospitals, academic institutions, and private pathology labs. In hospital settings, they often collaborate closely with dermatologists, surgeons, and oncologists, providing integrated care for patients with complex skin conditions.
In private labs, dermatopathologists might receive samples from dermatologists practicing across a region. These labs often have advanced equipment and can perform additional tests, such as immunohistochemistry and molecular diagnostics, which can aid in difficult or rare diagnoses.
Some dermatopathologists also split their time between laboratory work and teaching or research. In academic centres, they may contribute to medical education and clinical studies, helping to develop new diagnostic techniques and expand the knowledge base of skin pathology.
9. What does a dermatopathology report include?
A dermatopathology report typically includes a description of the biopsy specimen, a microscopic diagnosis, and relevant clinical comments. It begins with information about the type of sample received, such as punch, shave, or excisional biopsy, and its anatomical location on the body.
The heart of the report is the histopathological diagnosis. This section explains what was observed under the microscope, including the types of cells present, any abnormalities, and whether any signs of infection or malignancy were found. If cancer is detected, the report will also include important features like margins and depth of invasion.
Finally, the report may contain comments that correlate the findings with the clinical context, helping the treating dermatologist understand the significance of the results. In more complex cases, the dermatopathologist might also suggest further testing or offer a differential diagnosis to consider.
10. Are dermatopathologists involved in treatment decisions?
Although dermatopathologists don’t treat patients directly, their input is instrumental in shaping treatment decisions. By providing accurate and detailed diagnoses, they help dermatologists choose the most appropriate course of action. This could range from prescribing medication to performing additional surgery or referring the patient to a specialist.

Their reports often contain guidance that helps clinicians decide on next steps. For instance, if a skin cancer is diagnosed and the margins are not clear, the report may recommend a wider excision. In cases of autoimmune or inflammatory disease, the report may hint at a particular cause that needs to be addressed with targeted therapies.
So, while dermatopathologists aren’t on the front lines of patient care, they’re a crucial part of the clinical team. Their behind-the-scenes work ensures that decisions made by dermatologists are backed by solid, evidence-based diagnoses.
11. Can dermatopathologists diagnose non-cancerous skin conditions?
Absolutely. In fact, a large portion of a dermatopathologist’s work involves diagnosing non-cancerous conditions. These include inflammatory skin diseases like eczema, psoriasis, lichen planus, and dermatitis. Each of these conditions has specific microscopic features that help confirm or rule out a clinical diagnosis.
For patients with chronic or unusual skin rashes that don’t respond to standard treatments, a biopsy reviewed by a dermatopathologist can be extremely helpful. It can confirm the nature of the condition and guide more effective treatment options, reducing trial and error in managing symptoms.
Moreover, dermatopathologists can detect signs of infections, autoimmune diseases, and genetic skin disorders. Their findings often provide reassurance when no serious disease is present, or they help identify subtle conditions that might otherwise be overlooked in a standard clinical examination.
12. How accurate are dermatopathology diagnoses?
Dermatopathology is considered one of the most precise diagnostic fields in medicine. The combination of detailed visual analysis, specialised stains, and advanced techniques like immunofluorescence and molecular testing ensures high diagnostic accuracy. However, no test is perfect, and sometimes additional information or repeat biopsies may be needed.
Accuracy also depends on the quality of the biopsy and the clinical information provided by the referring doctor. A well-taken biopsy with clear clinical notes allows the dermatopathologist to interpret the findings more effectively and issue a more definitive diagnosis.
When uncertainty remains, dermatopathologists often collaborate with their peers or refer to academic centres for second opinions. This collaborative approach ensures patients benefit from the most informed and accurate diagnosis possible, even in the most complex cases.
13. Do dermatopathologists perform biopsies?
Dermatopathologists typically do not perform biopsies themselves. Instead, they examine tissue samples that have been collected by dermatologists, surgeons, or other healthcare professionals. Their work is focused on the microscopic analysis and interpretation of those samples.

However, some dermatologists who are dual-certified in dermatopathology may perform biopsies and then analyse the tissue themselves. This is less common but can be beneficial in certain clinical settings where immediate feedback is needed.
In general practice, though, the roles are clearly divided: the dermatologist manages the patient and collects the biopsy, while the dermatopathologist analyses the sample and provides the diagnostic report that guides treatment.
14. Can dermatopathologists identify rare skin diseases?
Yes, identifying rare and complex skin diseases is one of the strengths of dermatopathologists. Their specialised training allows them to recognise unusual cellular patterns and histological features that may be missed by general pathologists. This skill is particularly important when patients present with conditions that don’t respond to typical treatments or have unclear clinical presentations.
For example, rare autoimmune conditions like pemphigus vulgaris or cutaneous T-cell lymphoma require a high level of diagnostic skill. These diseases often mimic more common conditions in their early stages, but under the microscope, they reveal distinct features. Dermatopathologists use advanced staining techniques and molecular tools to confirm these rare diagnoses with confidence.
When a rare disease is suspected, the dermatopathologist may also recommend additional tests or consultations with other specialists. This collaborative approach ensures that patients receive the most accurate diagnosis and a tailored treatment plan, even when facing a complex or unfamiliar skin condition.
15. How do dermatopathologists work with other doctors?
Dermatopathologists work closely with dermatologists, surgeons, oncologists, and general practitioners to ensure seamless patient care. When a tissue sample is submitted, it’s usually accompanied by clinical information, images, and the doctor’s initial impressions. This helps the dermatopathologist interpret the sample in the right context.
After the analysis, the dermatopathologist produces a report, which is sent back to the referring doctor. If the findings are complex or unexpected, there may be further discussions, either through written notes or direct consultations. This two-way communication helps clarify the diagnosis and allows the clinical team to plan the most appropriate course of treatment.
In multidisciplinary team meetings, particularly in cancer centres, dermatopathologists often present their findings and discuss cases with the wider clinical team. Their insights can significantly influence decisions about surgery, medication, or referral to specialised services, making them key players in the broader healthcare network.
16. Are dermatopathologists involved in skin allergy testing?
While dermatopathologists are not directly involved in conducting allergy testing such as patch tests or prick tests, they do play a role when skin reactions require histological evaluation. If a rash or skin irritation is severe or persistent, a dermatologist may take a biopsy to rule out other conditions or confirm a diagnosis related to allergies.
When analysing these biopsies, the dermatopathologist looks for patterns consistent with allergic contact dermatitis or other hypersensitivity reactions. These microscopic clues help the dermatologist determine whether the issue is allergy-related or due to another inflammatory process.

So, while dermatopathologists don’t administer or interpret skin allergy tests themselves, they’re crucial in identifying underlying allergic reactions when standard testing or clinical observation isn’t enough to confirm a diagnosis.
17. What role does a dermatopathologist play in diagnosing autoimmune skin disorders?
Autoimmune skin conditions, such as lupus erythematosus or dermatomyositis, can be difficult to diagnose clinically. Dermatopathologists are essential in these cases because they can identify specific cellular changes and patterns of inflammation that suggest an autoimmune origin. Special stains and immunofluorescence are often used to detect immune deposits within the skin layers.
These findings are particularly valuable when a patient presents with systemic symptoms and skin involvement. For instance, in lupus, the skin biopsy might show basal cell degeneration and immune complex deposition, which support the diagnosis and may influence treatment choices such as immunosuppressive medications.
By working closely with dermatologists and rheumatologists, dermatopathologists help ensure that patients receive an accurate diagnosis and a multidisciplinary care plan. Their expertise allows them to distinguish between similar-looking autoimmune and non-autoimmune conditions, which is critical in avoiding misdiagnosis.
18. Can a dermatopathologist’s findings ever be inconclusive?
Yes, there are times when a dermatopathologist’s findings are inconclusive. This can happen for several reasons—such as if the biopsy sample is too small, poorly preserved, or taken from an area that doesn’t capture the disease process fully. In other cases, the histological features may overlap between multiple potential diagnoses.
When results are inconclusive, the dermatopathologist will usually suggest further steps. This might include repeating the biopsy, taking a sample from a different area, or ordering additional tests such as immunohistochemistry or molecular studies. These follow-up actions help clarify the diagnosis and avoid unnecessary treatment based on uncertain findings.
It’s important to remember that medicine is not always black and white. Even with the most advanced tools, some conditions defy immediate classification. In such cases, a thoughtful, collaborative approach between the dermatologist and dermatopathologist ensures the patient continues to receive careful and appropriate evaluation.
19. How can patients be reassured about the quality of dermatopathology?
Patients can feel reassured knowing that dermatopathologists are highly trained and often work under strict quality assurance protocols. In many settings, dermatopathology labs are accredited and participate in regular audits and proficiency testing to maintain high standards. This ensures that diagnoses are not only accurate but consistently reliable.
Furthermore, complex or high-risk cases often undergo a second review, either within the same lab or at a specialist centre. This peer-review process adds another layer of certainty, especially for diagnoses involving cancer or rare skin diseases. In academic or teaching hospitals, cases may also be reviewed in group settings with senior consultants present.
If patients have concerns or want more information, they are encouraged to ask their dermatologist about the biopsy results and whether a dermatopathologist reviewed the sample. Transparency in communication and the involvement of highly skilled professionals help build trust in the diagnostic process.
Final Thoughts
Dermatopathologists might work behind the scenes, but their contributions are central to the accurate diagnosis and treatment of countless skin conditions. From identifying cancer at its earliest stages to helping decode complex autoimmune diseases, these specialists provide clarity in situations where visual assessments alone fall short. Their collaboration with dermatologists and other clinicians ensures that patients receive the most appropriate and effective care.
Understanding the role of a dermatopathologist can offer reassurance during what may be a confusing or stressful diagnostic process. Their findings form the backbone of many treatment plans, helping doctors make informed choices that directly affect patient outcomes. Although most people may never meet their dermatopathologist face-to-face, the impact of their work is significant and lasting.
As with all aspects of healthcare, open communication between patients, dermatologists, and dermatopathologists strengthens trust and improves results. Knowing that a dedicated expert is analysing your biopsy with care and precision can bring peace of mind—and ultimately lead to better, more personalised treatment. If you’re concerned about any skin issue, you can contact us at The London Dermatology Centre to book a consultation with one of our expert private dermatologists.
