Eczema, also known as atopic dermatitis, is a common inflammatory skin condition that affects individuals of all ages. However, the presentation, triggers, and management can vary significantly between children and adults. Understanding these differences is crucial—not only for effective treatment but also for improving long-term outcomes and quality of life.
Eczema in Children: A Common Start
Eczema is frequently seen in children under the age of five, often making its first appearance in infancy. For many families, it can be an early and distressing introduction to chronic skin conditions, especially when the child is too young to communicate their discomfort. The condition is not only prevalent but also tends to run in families, especially where there is a history of allergies, asthma, or hay fever, indicating a strong genetic component.
The visibility of eczema in children, particularly in exposed areas like the face and arms, can cause considerable concern for parents. It may begin as dry patches or areas of redness that worsen with scratching. These patches can flare up intermittently, often triggered by changes in the weather, illness, or contact with irritants. The unpredictable nature of these flare-ups can make it difficult for parents to manage the condition consistently, adding to the emotional burden.
While some children outgrow eczema by adolescence, others may continue to experience symptoms into adulthood. Even in cases where the skin clears up, there can be lingering sensitivity that makes the child prone to other forms of dermatitis later in life. This early exposure to skin inflammation can also increase the likelihood of developing other allergic conditions, reinforcing the importance of early recognition and effective treatment strategies.
Presentation in Children
The way eczema presents in children can vary depending on age, with the distribution of affected areas changing as the child grows. In babies, it commonly affects the cheeks, forehead, and scalp, creating patches of red, inflamed skin that may be accompanied by oozing or crusting. These areas are particularly vulnerable because infants frequently rub or scratch them, even unintentionally, due to the intense itchiness that comes with the condition.
As children become toddlers and begin to move around more, eczema tends to migrate to areas that flex or crease, such as the inner elbows, behind the knees, and around the ankles and wrists. This change in location is often due to increased friction and sweating in these regions, which can aggravate the skin. The chronic irritation caused by persistent scratching may lead to thickened, roughened patches—a response known as lichenification—which makes the skin more difficult to treat and more prone to recurrent flare-ups.

Eczema in children can also become a vicious cycle: the itch leads to scratching, which breaks the skin and invites bacteria, resulting in infection and more inflammation. This cycle is particularly problematic at night, as itching can interfere with sleep, leading to fatigue, irritability, and challenges with concentration and learning. In this way, eczema affects more than just the skin; it can influence a child’s overall development and wellbeing, making effective management even more crucial.
Triggers and Causes
In children, eczema often arises from a combination of genetic predisposition and environmental exposure. Children with a family history of atopic conditions are significantly more likely to develop eczema themselves. This hereditary link suggests that the skin barrier in these individuals may be inherently weaker, allowing allergens and irritants to penetrate more easily and cause inflammation. In some children, a specific gene mutation affecting the skin barrier protein filaggrin has been identified, further supporting the genetic basis of the condition.
Environmental factors play a major role in triggering and aggravating eczema symptoms. Everyday substances such as soaps, bubble baths, laundry detergents, and even certain fabrics can irritate the skin and lead to flare-ups. Allergens in the home environment—like pet dander, house dust mites, and pollen—can also provoke symptoms, especially in children who already have a sensitised immune system. Additionally, fluctuations in temperature or humidity can make the skin more reactive, contributing to seasonal variations in eczema severity.
Food sensitivities may also play a part, particularly in younger children, although not all children with eczema have food allergies. Common culprits include cow’s milk, eggs, peanuts, and wheat, but these vary widely from case to case. It’s important that dietary triggers are investigated carefully under medical supervision, as unnecessarily restrictive diets can affect a child’s growth and nutrition. As children grow and their immune systems mature, their skin may become less reactive, but this is not guaranteed—some may continue to experience eczema well into adolescence and beyond.
Eczema in Adults: Persistence or Onset?
Eczema in adults can follow one of two main paths—either continuing from childhood or emerging for the first time in adulthood. For those who have lived with eczema since an early age, flare-ups may become less frequent over time, but the condition can still persist, particularly during times of stress or environmental change. Others may find that their eczema goes into remission during adolescence only to reappear unexpectedly later in life, often more resistant to treatment than before.
Adult-onset eczema, on the other hand, can be particularly frustrating because it arrives without warning and may not be immediately recognised for what it is. Individuals who develop eczema later in life might initially mistake it for dry skin or an allergic reaction, delaying appropriate treatment. In many cases, the cause may be multifactorial, involving a combination of immune response, environmental exposure, and underlying health issues. It is also more likely to become chronic, requiring long-term management rather than short-term relief.
The emotional impact of developing eczema as an adult can be considerable. Unlike children, who often receive support from caregivers and healthcare providers from the outset, adults may feel isolated in managing their condition, especially if it affects their appearance or interferes with daily life. Many report feeling self-conscious, particularly when lesions are visible on the face or hands. This, coupled with the unpredictable nature of flare-ups, can significantly affect confidence, relationships, and quality of life.
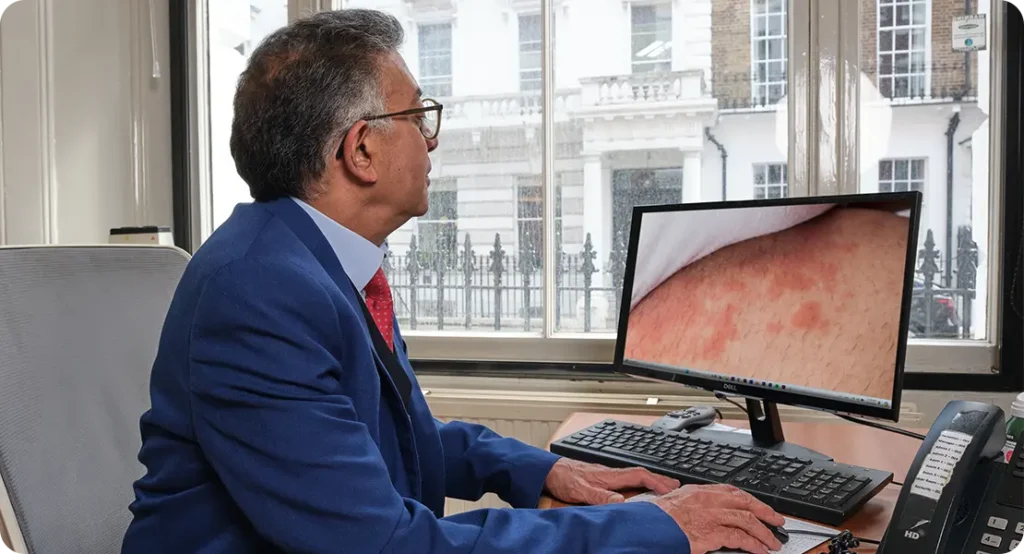
Presentation in Adults
The physical manifestation of eczema in adults tends to differ from the classic presentation seen in childhood. In adults, the condition often appears in more localised patches, especially on the hands, eyelids, face, and neck. These areas may develop a dry, rough texture and may crack or bleed during flare-ups. Unlike the bright red rashes commonly seen in children, adult eczema often results in a more muted or dusky tone due to repeated inflammation, which can also lead to skin thickening over time.

Another key feature of adult eczema is its chronicity. Rather than appearing in short-lived episodes, adult eczema may linger for months or even years, cycling through phases of flare and remission. The skin may become thickened, rough, or hyperpigmented due to long-standing inflammation and scratching. These changes can be particularly stubborn to reverse, even with ongoing treatment. In some cases, areas of the skin become permanently altered in appearance, leading to long-term cosmetic concerns.
Adults with eczema are also more susceptible to complications such as secondary infections. When the skin barrier is repeatedly compromised through scratching, bacteria such as Staphylococcus aureus can easily colonise the skin, leading to impetigo or cellulitis. In more severe cases, viral infections like eczema herpeticum can develop, requiring urgent medical attention. Additionally, chronic scratching may result in lichen simplex chronicus—a condition where the skin becomes leathery and deeply lined—adding another layer of complexity to treatment.
Triggers in Adulthood
The range of potential triggers for eczema tends to widen in adulthood, as individuals are exposed to more environmental, occupational, and lifestyle-related stressors. One of the most common culprits is prolonged exposure to irritants—such as harsh soaps, cleaning products, and solvents—particularly in professions that involve frequent hand washing or contact with chemicals. This repeated exposure can damage the skin barrier, leaving it vulnerable to inflammation and allergic reactions, especially on the hands and forearms.
Stress is another major contributor to adult eczema. The connection between psychological wellbeing and skin health is well-documented, and many adults report flare-ups during periods of emotional strain. Hormonal fluctuations—such as those experienced during pregnancy, menopause, or even the menstrual cycle—can also influence eczema severity. Unlike in children, where food triggers are more prominent, adult eczema is often more reactive to environmental and internal physiological changes.
Comorbid conditions play an important role in how eczema presents and progresses in adults. People with chronic health issues such as diabetes, obesity, or autoimmune disorders may find that their eczema is more difficult to control. Mental health conditions like anxiety and depression can also worsen symptoms, either by amplifying the perception of itch or by making it harder to adhere to treatment routines. Therefore, successful management often requires a multi-faceted approach that addresses not just the skin, but the individual’s overall health and lifestyle.
Why the Differences Matter
Recognising the distinctions between eczema in children and adults is not just helpful—it is essential to effective clinical management. The condition evolves with age, and what works for a toddler may not be suitable for an adult with the same diagnosis. Without an understanding of these variations, there is a risk of misdiagnosis or under-treatment, which can lead to prolonged discomfort and unnecessary complications.
For healthcare providers, age-specific knowledge helps guide appropriate investigations and treatment strategies. A child with recurrent eczema may need assessment for food allergies or environmental triggers, whereas an adult might require patch testing to rule out contact allergens or an evaluation for underlying chronic illnesses. This tailored approach ensures that treatment is both safe and relevant to the patient’s life stage and health status.
From the patient’s perspective, understanding how eczema changes with age can empower individuals and families to manage the condition more effectively. It can reduce anxiety about flare-ups, foster realistic expectations, and promote adherence to treatment. Additionally, it enables patients and caregivers to anticipate potential challenges—such as skin infections or psychological effects—and to take early action when needed.
Tailored Treatment Approaches
Treatment strategies for eczema must take into account the age of the patient, the severity of the condition, and the broader context of their life and health. In children, therapy typically revolves around maintaining skin hydration with regular emollient use and managing flare-ups with mild to moderate topical corticosteroids. Consistency in skincare routines is key, and educating parents or caregivers is a crucial part of ensuring these routines are followed correctly.
Young children may also benefit from avoiding common irritants such as fragranced soaps, synthetic clothing, and overly warm baths. Preventive strategies are important, especially when children are too young to articulate their symptoms. Involving the whole family in eczema care can help build supportive habits that prevent triggers and reduce the emotional stress associated with chronic conditions in childhood.

In contrast, adults may require more intensive interventions, especially if the eczema is chronic, widespread, or resistant to basic treatments. Stronger topical therapies, oral medications such as corticosteroids or immunosuppressants, and newer biological treatments may be considered. Moreover, adults often need to make broader lifestyle adjustments—modifying their work environments, managing stress levels, and addressing co-existing health problems—to gain full control of their symptoms.
Psychological Impact
The psychological burden of eczema is often underestimated, yet it can significantly affect an individual’s quality of life. For children, visible eczema can become a source of teasing or exclusion, especially in school settings. They may develop anxiety about their appearance or frustration with the constant need for treatment. In severe cases, this emotional stress can contribute to behavioural issues or impact academic performance.
Parents, too, can experience psychological strain when managing a child’s eczema. Feelings of guilt, helplessness, or exhaustion are not uncommon, particularly during periods of persistent flare-ups. Sleep disruption—caused by the child’s night-time itching—can affect the entire household. Offering emotional support and reassurance to families is just as important as treating the skin itself, helping them feel less alone in dealing with the condition.
Adults with eczema often face different psychological challenges. The condition can interfere with work, social life, and intimate relationships, particularly when the skin is visibly affected or the itch becomes unbearable. The unpredictability of flare-ups may cause anxiety or embarrassment, and in some cases, people withdraw from social activities altogether. Addressing these issues through counselling, peer support, or integrated care can make a substantial difference in long-term outcomes.
Prognosis and Prevention
The long-term outlook for eczema varies depending on several factors, including age of onset, severity, and underlying causes. In many children, eczema improves with age, especially when managed proactively in the early years. Early intervention not only helps reduce flare-ups but may also limit the development of related conditions such as asthma or allergic rhinitis, known collectively as the atopic march.
Preventative care during childhood can lay the foundation for healthier skin in later life. Simple habits such as using fragrance-free skincare products, avoiding known allergens, and maintaining good skin hydration can make a big difference. In high-risk children—particularly those with a strong family history—paediatricians may recommend strategies such as early introduction of certain foods or regular dermatological monitoring to minimise long-term impact.
For adults, prevention focuses more on identifying and mitigating triggers, especially those related to lifestyle or occupation. Avoiding irritants, managing stress, and seeking early treatment for flare-ups can help prevent the condition from worsening. While eczema is rarely “cured” in adulthood, consistent care and self-awareness can reduce the frequency and intensity of symptoms, preserving both skin integrity and overall wellbeing.
Conclusion
Eczema is a dynamic condition that evolves with age, reflecting both the maturity of the immune system and the cumulative impact of environmental exposures and lifestyle factors. By recognising the distinct characteristics of eczema in children versus adults, healthcare providers, patients, and caregivers can adopt more effective, age-appropriate strategies for management and support. Ultimately, this tailored approach improves not just the skin—but the overall well-being of those affected. If you’re concerned about eczema, you can contact us at the London Dermatology Centre to book a consultation with one of our expert dermatologists who specialise in managing this condition.
