Artificial intelligence (AI) might sound like something from a sci-fi film, but it’s already making real changes in medicine — especially in dermatology. Whether it’s spotting a suspicious mole earlier or helping you manage chronic skin conditions more effectively, AI is quietly but powerfully reshaping how skin health is diagnosed, monitored and treated.
Smarter, Faster, and More Accurate Diagnosis
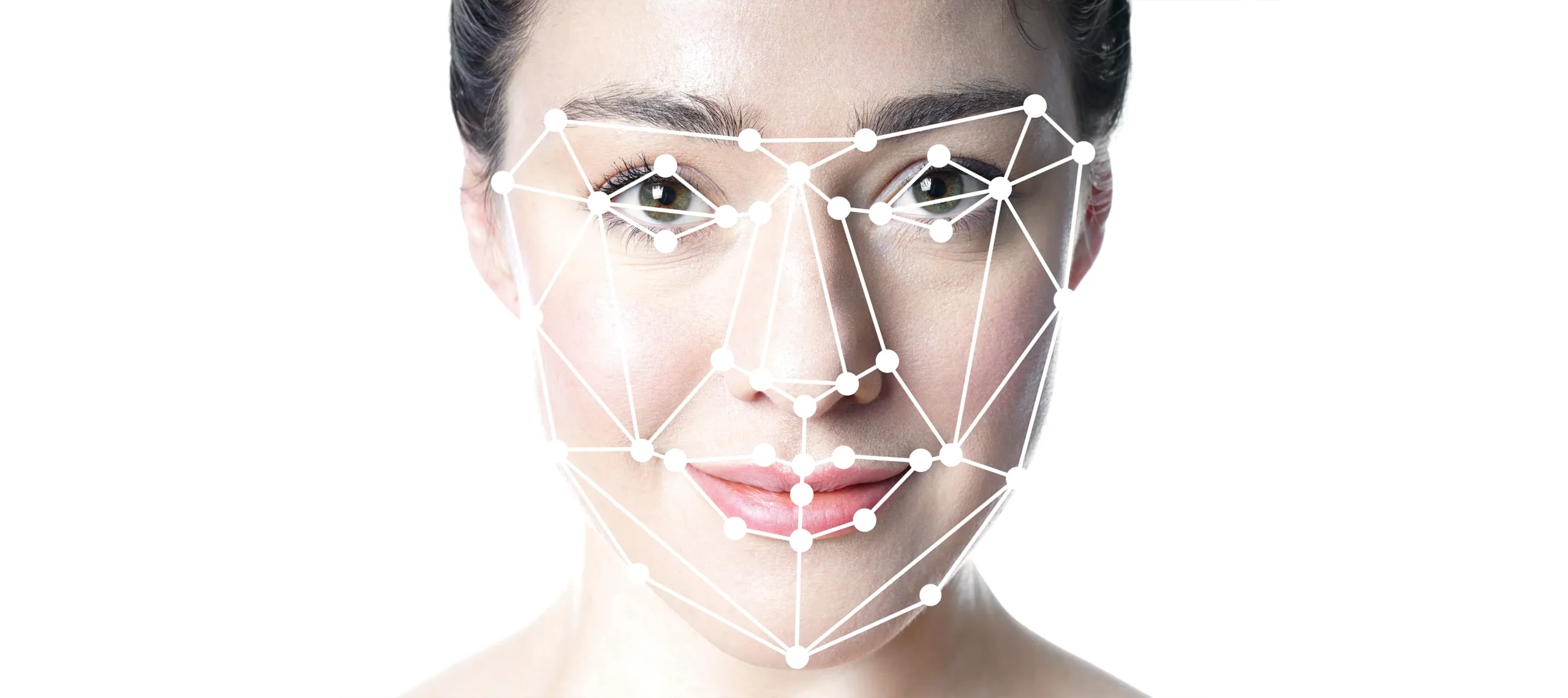
One of the most transformative ways AI is improving dermatology is through its role in diagnosing skin conditions more quickly and with impressive precision. When someone notices an unusual mole, rash, or lesion, timing can be critical — and that’s where AI-powered diagnostic tools shine. These systems can scan and interpret high-resolution images of the skin, offering an assessment within seconds. By doing so, they help identify which cases might need urgent attention and which are likely to be benign, reducing unnecessary worry and delays.

Behind the scenes, these AI models are trained on extensive image libraries — sometimes millions of clinical photographs — covering a wide range of skin tones, conditions, and disease stages. Through this training, the algorithms learn to distinguish fine visual cues that may be missed by the human eye, especially in very early or atypical presentations of disease. This is particularly useful in spotting malignant skin cancers such as melanoma, where early detection dramatically improves prognosis. Rather than replacing dermatologists, these tools function as intelligent assistants, offering an additional layer of insight to support clinical decisions.
One of the key advantages of AI in diagnosis is its consistency. While human interpretation can be influenced by fatigue, time pressure, or subjective judgement, AI systems deliver the same level of analysis every time. This can help reduce diagnostic errors, especially in fast-paced or under-resourced settings. As a result, patients receive more dependable outcomes, and clinicians can focus their time and expertise on complex or ambiguous cases where human interpretation remains vital.
In regions where access to dermatologists is limited, AI technology is already closing the gap. With the help of mobile devices or digital kiosks, trained healthcare workers or patients themselves can capture skin images, which AI can then analyse remotely. This helps prioritise urgent cases and ensures those who need specialist care are not left behind. As this technology becomes more accessible, it has the potential to revolutionise early skin disease detection globally, particularly in underserved areas where timely diagnosis has traditionally been a challenge.
Improving Screening and Catching Problems Earlier
AI is playing a crucial role in transforming how skin conditions are screened, shifting the focus from reactive to proactive care. Traditionally, skin cancer checks have largely depended on patients noticing something unusual and seeking a consultation. This reactive model often results in delays, especially when symptoms are subtle or go unnoticed. AI is changing this dynamic by enabling continuous, technology-driven monitoring that encourages earlier detection and intervention.
Mobile apps powered by AI are making self-screening more accessible than ever. Users can take photos of moles or lesions using their smartphone camera, and the app analyses them for signs of potential concern. Many of these tools allow individuals to track changes in the appearance of moles over time, providing reminders to recheck or prompting a visit to a doctor if something changes significantly. This creates a more active and engaged approach to skin health, even among those who may not regularly visit a dermatologist.

Beyond personal use, AI is being employed in clinical settings to identify patients who may require further investigation. By analysing large volumes of medical records, including previous dermatology notes and imaging, AI systems can flag individuals at higher risk based on their history. This is particularly valuable for people with chronic conditions, a family history of skin cancer, or those with a high number of atypical moles. By narrowing down who should be prioritised for screening, AI allows healthcare providers to focus resources more effectively.
AI-assisted screening is also closing the gap in remote and underserved regions where dermatologists are few and far between. Community health workers equipped with AI-enabled devices can conduct basic skin checks and transmit images for remote analysis. This model helps ensure early identification of serious conditions, even in populations that previously lacked access to routine dermatological care. As a result, more people are being screened earlier, when treatment is most effective.
Treatment That’s More Personal and Precise
AI is bringing a new level of precision to the treatment of dermatological conditions by enabling more tailored approaches based on individual characteristics. Conditions like acne, eczema, and psoriasis can vary dramatically from person to person — what works well for one individual might be ineffective or even harmful for another. AI tools help to untangle this complexity by analysing patterns in patient data to guide more informed treatment decisions.
By looking at a patient’s medical history, previous treatment responses, genetic information (where available), and even lifestyle factors, AI systems can help clinicians design treatment plans that are likely to be most effective for that specific individual. This avoids the common “trial and error” approach that often prolongs suffering and delays relief. AI can also draw from anonymised data across thousands of patients to identify which combinations of therapies have worked in similar cases, offering evidence-based recommendations.
Some AI tools are being developed to forecast how a patient might respond to particular medications before those treatments even begin. This predictive capability helps avoid adverse reactions or ineffective interventions, making the treatment journey safer and more efficient. For chronic skin conditions that may persist for years, this targeted approach is especially valuable, as it can help patients find relief faster and maintain better long-term skin health.
In cosmetic dermatology, AI is also influencing treatment planning by helping practitioners visualise outcomes more accurately. By modelling changes in pigmentation, texture, or inflammation, AI can help set realistic expectations and optimise aesthetic results. Altogether, this shift toward personalised dermatological care is empowering both patients and clinicians, ensuring that each treatment is as specific and effective as possible.
Making Clinics More Efficient
Dermatology clinics are often under pressure, with rising patient demand and limited resources leading to long wait times and stretched appointment slots. AI is stepping in to ease this burden by streamlining administrative processes and improving clinical efficiency. From appointment scheduling to managing electronic medical records, AI can handle many of the routine tasks that traditionally consume valuable clinician time.
One key area where AI is making a difference is in triage — determining which patients need to be seen most urgently. AI-powered systems allow patients to upload images and brief descriptions of their symptoms before their visit. These tools then assess the level of urgency based on the information provided, helping clinics organise their workflow more effectively. This ensures that serious cases are prioritised, while those with non-urgent concerns can be managed more flexibly.
In addition to improving how patients are booked and seen, AI is helping reduce the administrative load on dermatologists by generating draft clinical notes and treatment summaries. These tools use natural language processing to convert spoken or written input into structured documentation, which saves time without compromising accuracy. By reducing the clerical burden, dermatologists can spend more of their time engaging with patients and focusing on complex clinical issues.
AI is also enhancing inventory and resource management within dermatology practices. Predictive algorithms can monitor the usage of medical supplies, flag shortages before they happen, and suggest optimal stock levels based on historical data. Combined with improved patient flow and better time management, these efficiencies are allowing clinics to run more smoothly, deliver better care, and reduce unnecessary stress for both staff and patients.
What About the Risks?
1. Bias in Diagnostic Accuracy
As promising as AI may be for dermatology, one of the most significant concerns is that it may not serve all patients equally. Many AI tools are trained predominantly on image datasets that reflect lighter skin tones, simply because those images are more widely available in clinical archives. As a result, the system may struggle to recognise the same conditions when they appear on darker skin, where features can present differently. This discrepancy could lead to missed diagnoses or delayed treatment for people from underrepresented groups, worsening existing health inequalities.
Addressing this bias isn’t just a technical issue — it’s an ethical one. Without deliberate efforts to improve the diversity of training datasets, the benefits of AI in dermatology risk being skewed toward certain populations. Building inclusive models means actively sourcing images across a wide range of skin types, ensuring balanced representation of ethnic backgrounds, and continually testing the tools for fairness. Only then can AI become a force for reducing bias in dermatological care, rather than reinforcing it.
2. Gaps in Data Representation
Beyond skin tone, other forms of underrepresentation in AI training data can also create serious limitations. Many datasets are skewed toward certain age groups, genders, or geographic regions, which means that conditions affecting underrepresented demographics may be poorly understood by the algorithm. For instance, skin conditions in older adults or children may manifest differently than in the general adult population, yet these groups are often less well-represented in training data.
Additionally, diseases that are rare or more prevalent in specific parts of the world may not be adequately captured in mainstream datasets, leading to weak recognition or misclassification. For AI to be truly effective and equitable, it must be built on data that mirrors the diversity of the real world. This includes rare skin diseases, atypical presentations, and populations that may not frequently access healthcare. Without this breadth, AI will continue to have blind spots — and these gaps can have real clinical consequences.
3. Privacy and Data Security Concerns
AI in dermatology relies heavily on the collection and analysis of personal health data, often including high-resolution skin images, medical histories, and metadata that can be highly sensitive. If this information is not stored or handled correctly, it creates a serious risk to patient privacy. With cyber threats on the rise, any breach could expose confidential health records and images, eroding trust between patients and providers and potentially causing long-term harm.
To mitigate this risk, strong data protection measures must be built into every stage of AI development and deployment. This includes encrypted storage, strict access controls, transparent data usage policies, and compliance with data protection regulations like GDPR. Patients should be informed about how their data is being used, who has access to it, and how long it will be stored. Ethical AI development depends not only on technical accuracy but also on robust safeguards that prioritise patient confidentiality and consent.

4. The Limits of Artificial Intelligence
Despite its impressive capabilities, AI lacks the ability to fully understand the broader context of a patient’s experience. Dermatological conditions often go beyond the physical appearance of the skin — they can affect mental health, self-esteem, relationships, and quality of life. An AI tool may identify a rash or lesion with high precision, but it cannot grasp the emotional impact it has on a patient or tailor its recommendation with empathy and understanding.
Moreover, some conditions may require a nuanced interpretation of symptoms that considers cultural background, personal habits, or psychosocial stressors — elements an algorithm is not equipped to process. Human clinicians are trained not just to diagnose, but to listen, observe, and adapt their care to each individual’s needs. AI can support decision-making, but it should never replace the compassionate, flexible judgement that defines good medical practice.
5. The Need for Strong Oversight
As AI becomes more integrated into dermatology, there is a clear need for thorough regulation to ensure safety, reliability, and fairness. Without proper oversight, poorly tested tools could be released into clinical settings, potentially causing harm through misdiagnosis or inappropriate recommendations. Regulatory bodies must work closely with developers and healthcare professionals to establish clear standards for accuracy, bias testing, clinical validation, and ongoing monitoring.
In addition, there must be transparency in how AI systems reach their conclusions. Black-box models — where decisions are made without clear explanation — can undermine confidence and create legal or ethical challenges. Clinicians and patients alike should be able to understand how an AI tool arrived at its output and what data it was based on. With proper governance, AI can be held to the same high standards as any other medical device, ensuring that its benefits are delivered responsibly and equitably.
Summary
AI is making dermatology more accurate, accessible, and efficient. It’s helping doctors catch problems earlier, personalise treatments, and manage patient care more effectively. But at the heart of all this progress is the collaboration between human expertise and machine intelligence.
Dermatologists aren’t being replaced — they’re being supported by smarter tools that allow them to do what they do best: provide thoughtful, personalised care. As AI continues to evolve, its role in dermatology will only grow, improving outcomes and making high-quality skin care available to more people than ever before.