If you’ve been dealing with eczema for a long time, you’ll know it’s not just dry skin. It can be relentless—itchy, painful, inflamed, and often emotionally draining. For some, it’s a minor nuisance. But for others, chronic eczema can disrupt sleep, impact self-confidence, and seriously affect quality of life.
You may have tried moisturisers, over-the-counter creams, or been prescribed a steroid by your GP. And while these can help manage short-term symptoms, they often fall short when it comes to long-standing, complex eczema. That’s where a consultant dermatologist can make all the difference.
In this article, we’ll explore how dermatology specialists approach chronic eczema with advanced tools, expert insight, and a personalised treatment strategy—going far beyond the basics to help you regain control over your skin.
Why GP Treatments Aren’t Always Enough
GPs are a great first port of call, especially for mild or occasional eczema. They’ll often prescribe emollients and a short course of topical steroids to help settle flare-ups. But if your symptoms keep returning, are spreading, or simply aren’t responding to treatment, it may be time for a more detailed approach.
Chronic eczema isn’t always straightforward. There could be underlying allergies, contact sensitivities, or even environmental triggers you haven’t identified. Some people also develop a resistance to standard creams, or experience worsening symptoms when they try to reduce use.
GPs are limited by time, and their treatment options tend to follow generalised guidelines. This can mean they’re only able to offer surface-level solutions without digging deeper into what’s really driving your eczema. They may not have access to more advanced treatments or diagnostic tools that could uncover hidden causes or tailor your treatment more precisely.
In some cases, eczema can also mask or overlap with other skin conditions, which makes specialist input essential. If your skin isn’t improving—or if it’s affecting your sleep, work, or confidence—it’s worth getting an expert opinion. If you feel like you’re stuck in a loop of flares and prescriptions, seeing a consultant dermatologist could be the step that changes everything.
How Specialist Dermatologists Approach Chronic Eczema
When eczema becomes persistent, widespread, or unresponsive to standard treatments, it’s time to think beyond moisturisers and over-the-counter creams. Chronic eczema isn’t just a nuisance—it’s an ongoing condition that can significantly affect your comfort, sleep, work, and confidence. And while general practitioners do their best to help, they’re often limited by time, resources, and the scope of treatments they can offer.
That’s where a consultant dermatologist makes a real difference. Specialists in skin conditions, they bring a depth of knowledge and experience that allows them to dig deeper—identifying not only what’s causing your eczema, but why it keeps coming back. Their approach is more investigative, more precise, and more holistic.
Instead of simply managing flares as they arise, consultants focus on understanding the bigger picture—your lifestyle, your triggers, your full medical history—and designing a strategy that fits around you. They’re not just looking to calm the skin short term, but to help you achieve long-term stability.
In the next section, we’ll explore exactly how specialist dermatologists treat chronic eczema differently—from diagnostics and therapies to personalised care and flare prevention.
Advanced Diagnostic Testing (Including Patch Testing)
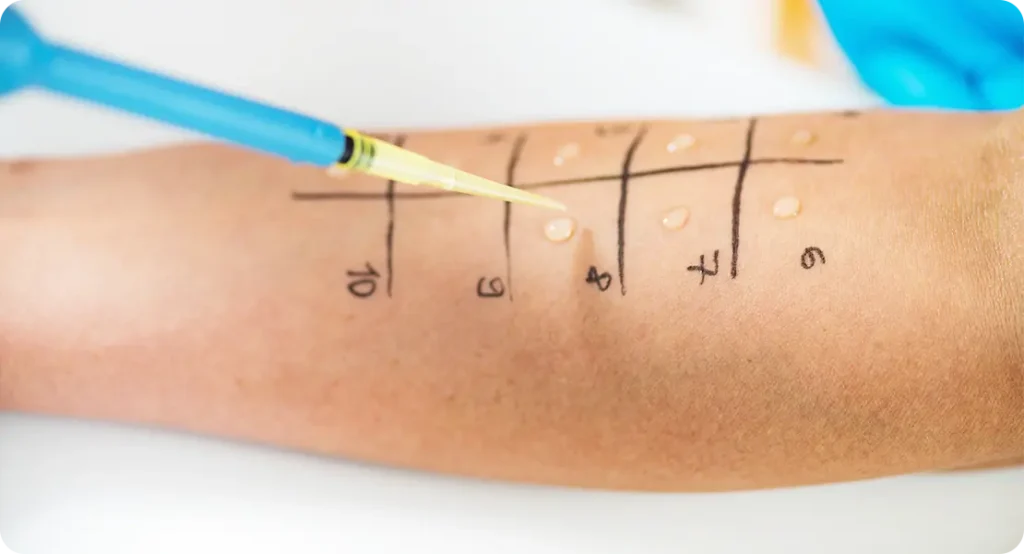
One of the key advantages of seeing a consultant dermatologist is access to advanced diagnostic tools. Patch testing is a prime example. This simple but effective method involves applying a series of allergens to your back under small patches, to see if your skin reacts over time under controlled conditions.
It’s incredibly useful for identifying contact allergens that might be fuelling your eczema—such as ingredients in skincare products, metals, clothing dyes, or preservatives. These aren’t always easy to pinpoint, and without this level of testing, many people continue exposing their skin to hidden irritants without realising it.
Beyond patch testing, your consultant may also assess for other underlying conditions, skin infections, or even refer you for blood tests if a systemic issue is suspected. The goal is to get a complete picture, so treatment isn’t just reactive—it’s informed, precise, and tailored to your skin’s specific needs.
Short-Term Immune-Modulating Therapy
For more severe cases, immune-modulating treatments may be used to reduce flare severity and give the skin time to recover. These are carefully selected and monitored by your consultant and are designed to calm the immune system’s overactivity, which lies at the root of chronic eczema.
Chronic eczema isn’t just a surface-level issue—it’s an immune-driven condition. The inflammation you see and feel is often the result of the body’s immune system reacting inappropriately, attacking healthy skin cells and disrupting the skin barrier. Immune-modulating therapy works by dialling down this overactive response, helping to break the cycle of persistent flares and skin damage.
These treatments are generally used for people who have tried topical approaches without success or whose eczema covers large areas of the body. They may be given orally or via injection, depending on the therapy type and severity of the condition. While they’re not always used long-term, they can be highly effective for stabilising eczema, especially when other methods have failed.
The benefit of being under a consultant dermatologist’s care is that you’re closely monitored throughout treatment. Your skin’s response, any side effects, and your general health will all be reviewed regularly, ensuring safety and effectiveness. Dosages can be adjusted, paused, or combined with other therapies to ensure the best possible outcome.
Importantly, immune-modulating therapies are often used alongside a wider treatment plan, not in isolation. This might include flare-control creams, barrier repair products, and trigger management advice. The result is a holistic strategy that doesn’t just treat the symptoms, but addresses the deeper mechanisms of eczema.
In private dermatology, this level of precision and support ensures that immune-based treatments are used confidently and appropriately, helping patients finally move towards longer-lasting skin stability.
Expert-Led Treatment for Flare Control
When it comes to treatment, consultant dermatologists have more tools at their disposal than most general practitioners. They understand the difference between occasional eczema and a complex, chronic case—and they treat it accordingly.
A tailored regimen might still include topical steroids, but used strategically, and often combined with steroid-sparing alternatives such as non-steroid anti-inflammatory creams. These are especially helpful for sensitive areas like the face or eyelids, and allow for long-term control without the same risks of skin thinning.
For more severe or widespread eczema, short courses of immune-modulating treatments may be recommended. These work by calming the underlying inflammation that causes flare-ups, giving the skin a chance to heal more effectively. These treatments are only prescribed when necessary and always under close supervision.
What sets consultants apart is the balance they strike—helping you control flares without relying too heavily on one type of product. They build a plan that works for your lifestyle, skin sensitivity, and long-term needs.
Personalised Advice for Reducing Triggers
Eczema is rarely just about what’s happening on the surface of your skin. Lifestyle factors—like stress, diet, fabric choices, and even your central heating—can all influence flare frequency and severity. A consultant dermatologist looks beyond the condition to understand the person living with it.

During your appointment, they’ll take the time to go through your history in detail: when your flares started, what seems to make them worse, what products you use daily, and how your environment may be contributing. From there, they’ll help you identify your unique triggers and offer realistic ways to avoid or minimise them.
This could include recommending gentler skincare alternatives, changing how and when you moisturise, or offering stress management strategies if emotional triggers are a factor. No two eczema patients are the same, and this kind of tailored advice can have a massive impact on long-term skin health.
Lifestyle and Environmental Trigger Assessment
One of the most valuable aspects of seeing a consultant dermatologist for chronic eczema is the opportunity to explore your personal triggers in detail. While eczema is often treated as a purely skin-related issue, many flare-ups are influenced by what’s happening around you—and even within you. Stress, diet, heat, certain fabrics, harsh soaps, allergens, and skincare ingredients can all play a role in worsening symptoms. A consultant takes time to ask the right questions and uncover what’s actually contributing to your flare-ups, rather than just treating the aftermath.
This kind of assessment is deeply personalised. You’ll likely discuss your daily routine, the products you use, your home and work environments, and any recent changes that might be linked to worsening skin. In some cases, patch testing or allergy testing may be recommended to pinpoint specific irritants. The result? You walk away with not just treatment, but knowledge and strategies to reduce flare frequency—things like choosing the right moisturisers, adjusting laundry habits, or managing emotional stress. It’s a proactive, empowering approach that puts you back in control. Because the more you understand your triggers, the better chance you have of keeping your eczema calm, consistently.
Long-Term Monitoring and Follow-Up
Chronic eczema isn’t a condition you fix once and forget—it’s a journey that requires regular adjustment, patience, and consistent care. That’s why long-term monitoring and follow-up with a consultant dermatologist are so important. When you’re under ongoing specialist care, your treatment doesn’t just stop after one prescription. You’ll have the benefit of review appointments where your progress is tracked, treatments are reviewed, and any changes to your skin are responded to quickly and effectively.
Over time, your skin’s needs may shift. Stress levels, hormones, environmental conditions, or even lifestyle changes can affect how your eczema behaves. What worked brilliantly last year might not work the same today—and that’s completely normal. With regular follow-ups, your consultant can tweak your treatment plan, step things up during flare periods, or safely reduce medication when your skin improves.
This continuity of care also allows your dermatologist to catch early signs of complications like infections, steroid overuse, or skin thinning, and address them early. In short, long-term monitoring is the difference between reactive care and proactive management. It’s how you move from crisis control to real confidence—and maintain healthy skin for the long run.
Why Choose Consultant Dermatology for Eczema?
So, what’s the real benefit of seeing a consultant dermatologist? In short—specialist care means better outcomes.
Here’s what you can expect from private dermatology treatment:
- Faster access to appointments (no waiting months for a referral)
- Longer consultations to understand your full health and skin history
- Comprehensive assessments including patch testing and advanced diagnostics
- Access to specialist-only treatments
- A personalised, adaptable care plan
- Ongoing support that evolves with your skin
When you’re living with chronic eczema, quick fixes and generic advice often don’t go far enough. A consultant dermatologist brings not only clinical expertise but a deep, day-to-day understanding of how eczema behaves and how it impacts your life. They won’t just focus on your current flare—they’ll look at patterns, triggers, past treatments, and how your skin reacts over time.
This level of care also brings reassurance. You’re not left second-guessing whether your cream is too strong, or if your flare is a sign of something more serious. With regular follow-ups and access to tailored treatments, you’re supported throughout the ups and downs. Your care evolves with your skin, rather than being fixed around a single prescription.
You’ll also gain access to treatments and monitoring that go beyond standard GP offerings, such as non-steroidal alternatives, long-term flare management strategies, and lifestyle coaching for ongoing control. Your treatment isn’t static—it’s active, responsive, and designed for long-term success.
And perhaps most importantly, you’ll feel heard. In private dermatology, there’s time for proper discussion, personalised planning, and an approach built around your goals—not just symptom relief. Rather than a one-off prescription, you’ll get a roadmap for lasting skin health and renewed confidence.
How to Choose a Consultant Dermatologist to Treat Chronic Eczema
Choosing the right consultant dermatologist to manage your chronic eczema is an important step toward getting the long-term relief and personalised care you deserve. Start by looking for someone who is fully GMC-registered and on the specialist register in dermatology—this confirms they’ve undergone the necessary training and are recognised by official medical bodies. It’s also helpful to find a dermatologist who has specific experience with eczema and other inflammatory skin conditions, as this ensures a deeper understanding of the complexities involved.
Next, consider the clinic’s approach to care. Chronic eczema isn’t just about prescribing creams—it requires a holistic and often multi-layered treatment plan. Look for consultants who offer comprehensive assessments, including allergy testing or patch testing, as well as long-term treatment strategies rather than one-off prescriptions. Reviews or patient testimonials can also offer insight into the consultant’s bedside manner and level of patient support.
Location and accessibility matter too, especially if follow-up appointments are needed regularly. Many private dermatologists offer virtual consultations alongside in-person care, which can be helpful for ongoing management. Lastly, choose someone you feel comfortable talking to. Managing eczema is a journey, and having a consultant who listens, explains clearly, and tailors treatment to your life—not just your skin—can make a world of difference.
How Long Does It Take to Treat Chronic Eczema with a Consultant Dermatologist?
The timeline for treating chronic eczema varies from person to person, but with a consultant dermatologist, the process typically moves more efficiently and with greater precision. In many cases, patients begin to see improvement within a few weeks of starting a tailored treatment plan. This is because consultants can quickly identify the most effective combination of therapies, whether that includes specialist creams, immune-modulating treatment, or lifestyle adjustments.
However, managing chronic eczema is rarely a one-off fix. Treatment is often ongoing and may take several months to stabilise the skin fully—particularly if the condition has been left untreated or poorly managed for years. Consultants also focus on long-term control, meaning your care will evolve through follow-up appointments to ensure sustained results and minimal flare-ups.

If allergy testing or patch testing is needed, that process alone can take a few weeks to complete and analyse before adjustments are made. But the benefit is a more accurate, long-term plan that helps prevent flare triggers from being overlooked.
Ultimately, while there’s no universal timeline, patients under consultant-led care typically reach clearer, calmer skin far more quickly—and with fewer relapses—than those relying on short-term GP support alone.
Ready to Take Control of Your Eczema?
If you’re tired of repeating the same treatments and getting the same results, it may be time to take a different path. Consultant dermatology offers a deeper, more proactive approach to managing eczema—especially when it’s chronic, complex, or just not getting better.
Unlike standard care, where you may feel like you’re starting from scratch at every appointment, specialist dermatology provides consistency, clarity, and a structured plan. You’ll be treated by someone who sees eczema cases every day and understands the frustration of unpredictable flares, sleepless nights, and the emotional weight that often comes with them. They don’t just treat symptoms—they look for the patterns, triggers, and hidden causes behind them.
With expert support, tailored treatment, and the right diagnostic tools, long-term control really is possible. You don’t have to settle for flare-up after flare-up. You can move forward—with clearer skin, better comfort, and a plan that finally works for you.
If you’re concerned about eczema, you can contact us at The London Dermatology Centre to arrange a private consultation with one of our expert dermatologists.
The first step is simple: book a consultation. From there, you’ll begin a journey toward healthier skin, guided by someone who’s committed to helping you regain confidence, comfort, and control.
