Dark patches or uneven skin tone can appear for many reasons and it’s not always easy to tell what’s causing them. You may notice brown or greyish marks developing on your cheeks, forehead, or other parts of your face or body, leading to frustration or self-consciousness. But not all pigmentation issues are the same, and that’s where things get tricky.
Two of the most common types of pigmentation are melasma and post-inflammatory hyperpigmentation, but they’re often confused with one another. While they may look similar on the surface, they differ in causes, behaviour, and how they respond to treatment. Melasma is typically triggered by hormonal changes and is notoriously stubborn, while other forms of hyperpigmentation can result from acne, sun exposure, or skin trauma and often respond more quickly to skincare treatments.
Understanding the root cause of your skin discolouration is crucial. Using the wrong treatment especially in the case of melasma can worsen the condition or lead to unwanted side effects. That’s why dermatologists place a strong emphasis on accurate diagnosis before recommending any pigmentation therapies.
In this guide, we’ll walk you through the key differences between melasma and other forms of hyperpigmentation. You’ll learn how to identify the symptoms, understand what might be triggering your skin changes, and discover why professional diagnosis and tailored treatment matter more than you might think.
What Is Hyperpigmentation?
Hyperpigmentation is a broad dermatological term that refers to patches of skin that appear darker than the surrounding areas. This darkening occurs when an excess amount of melanin the pigment responsible for skin, hair, and eye colour is produced and deposited unevenly in the skin. It’s not a condition in itself but rather a symptom of an underlying cause or trigger. Hyperpigmentation can vary in size and severity, from small dark spots to widespread areas of discolouration. These changes can develop gradually or appear suddenly, depending on the cause.
Some of the most common causes of hyperpigmentation include:
- Sun exposure: Ultraviolet (UV) rays stimulate melanin production, which can lead to sunspots (also called solar lentigines) or uneven skin tone, especially on frequently exposed areas like the face, shoulders, and hands.
- Inflammation: Skin trauma such as acne breakouts, eczema, psoriasis, or even minor cuts and burns can result in post-inflammatory hyperpigmentation (PIH), where the healing area becomes darker than the surrounding skin.
- Hormonal changes: Fluctuations in hormones especially oestrogen and progesterone can increase melanin production, contributing to conditions like melasma.
- Skin injuries: Burns, friction, waxing, or cosmetic procedures that irritate the skin can all lead to darkened patches during the healing process.
- Certain medications: Some drugs, including antibiotics, chemotherapy agents, and antimalarials, can cause hyperpigmentation as a side effect.
Hyperpigmentation can affect people of all skin types, but it is especially common in individuals with darker skin tones, where melanin activity is naturally higher. It can appear anywhere on the body, including the face, neck, back, hands, and even in areas with minimal sun exposure.
While it’s not usually harmful, hyperpigmentation can be distressing for cosmetic reasons and understanding the type and cause is key to finding the right treatment.
What Is Melasma?

Melasma is a specific type of hyperpigmentation that typically develops as a result of hormonal fluctuations, making it distinct from other causes of skin discolouration. It’s characterised by patches of brown or grey-brown pigmentation that usually appear on the face, particularly in areas frequently exposed to the sun.
Unlike other forms of pigmentation, melasma is known for its symmetrical distribution meaning it often appears evenly on both sides of the face. Common areas affected include the cheeks, forehead, upper lip, bridge of the nose, and occasionally the jawline.
Key features of melasma:
- Primarily affects women, especially during periods of hormonal change such as pregnancy (where it’s often referred to as the “mask of pregnancy” or chloasma), or while using oral contraceptives or undergoing hormone replacement therapy (HRT).
- Presents as large, flat patches of pigmentation rather than small individual spots.
- The colour tends to be brown or grey-brown, and the edges are usually well defined but not sharp.
- UV exposure and heat can make melasma worse even mild sun exposure without visible burning can trigger or deepen patches.
Melasma can be persistent and notoriously difficult to treat, especially if underlying triggers like hormone fluctuations or sun exposure are not addressed. While it doesn’t cause any physical harm, the impact on self-esteem and quality of life can be significant.
Because melasma does not always respond well to typical over-the-counter pigmentation treatments, dermatologists often recommend a specialised approach including prescription creams, medical-grade sun protection, gentle procedures, and sometimes a review of hormonal health.
Managing melasma often requires patience, consistency, and a long-term skincare plan, as flare-ups can occur even after successful treatment.
Main Differences Between Melasma and Other Hyperpigmentation
Although melasma falls under the umbrella of hyperpigmentation, it behaves quite differently from other types of dark spots or discolouration. Understanding these differences is crucial when it comes to diagnosis and selecting the right treatment approach.
The underlying cause is one of the primary distinctions. Melasma is strongly influenced by hormonal changes such as those that occur during pregnancy, with oral contraceptive use, or hormone replacement therapy and is often worsened by UV exposure and even heat. In contrast, other forms of hyperpigmentation are more commonly triggered by external factors, such as sun damage, post-inflammatory responses to acne or eczema, or trauma to the skin like cuts or burns. The location of the discolouration also helps differentiate the two. Melasma almost exclusively appears on the face, particularly the cheeks, forehead, bridge of the nose, and upper lip. It often forms a symmetrical pattern across both sides of the face. On the other hand, other hyperpigmentation types can develop anywhere on the body, including the back, chest, arms, or legs essentially any area affected by inflammation or sun exposure.
When it comes to appearance, melasma tends to present as broad, flat patches that are either brown or grey-brown in colour, and often have a blurred or soft-edged outline. Other pigmentation issues, such as post-inflammatory hyperpigmentation or sunspots, typically appear as smaller, more irregularly shaped dark spots and can range in shade from light brown to deep black, depending on skin tone and depth. Triggers vary significantly as well. Melasma is often activated or worsened by hormonal shifts and UV radiation, making it more persistent and unpredictable. Meanwhile, other forms of hyperpigmentation are commonly triggered by acne, skin injuries, sunburn, or certain medications. Finally, there’s a key difference in treatment response. Melasma is typically slow to fade and can relapse easily if not managed carefully. It requires ongoing care, strict sun protection, and often prescription-based treatments. In contrast, most other hyperpigmentation types tend to respond faster to topical products, chemical peels, or laser treatments though they still benefit from professional supervision to avoid complications like post-inflammatory pigmentation.
In short, while melasma and other hyperpigmentation may look similar to the untrained eye, they are distinct in cause, behaviour, and treatment needs which is why a dermatologist’s diagnosis is so important.
Diagnosis: Why It Matters
When it comes to skin pigmentation issues, getting the right diagnosis is not just helpful it’s essential. That’s because melasma and other types of hyperpigmentation often require very different treatment strategies, and using the wrong approach can actually make the condition worse.
For example, post-acne pigmentation a form of post-inflammatory hyperpigmentation often responds well to chemical exfoliants like glycolic acid or salicylic acid peels. These treatments speed up skin cell turnover and help fade dark spots over time. However, applying the same exfoliating acids to melasma-prone skin especially without professional supervision can irritate the skin, increase inflammation, and worsen pigmentation. Melasma is far more sensitive to external triggers and requires a gentler, more tailored approach.
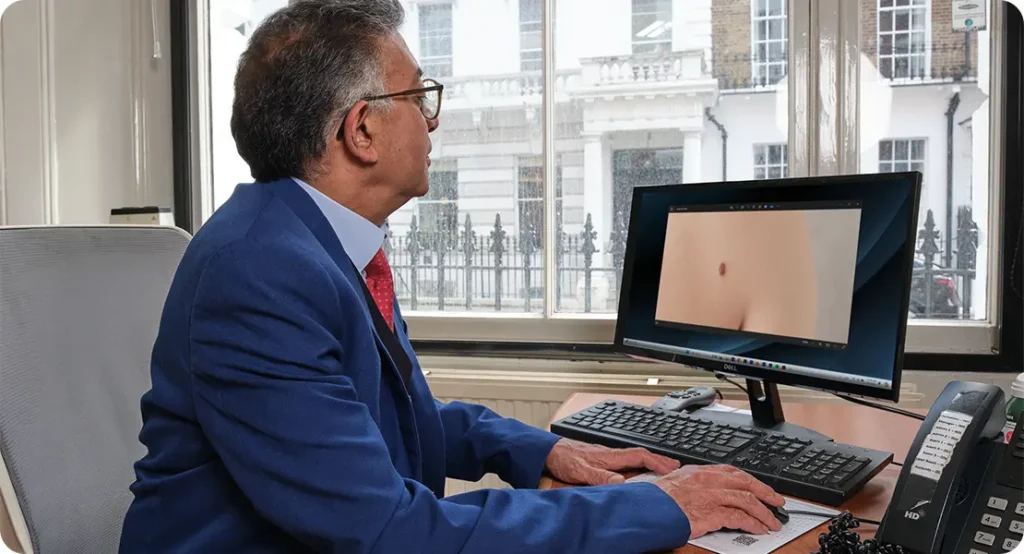
This is why dermatologist-led diagnosis is key. Specialists are trained to distinguish between different types of pigmentation by looking at factors like location, shape, colour, patient history, and more. They often use a combination of diagnostic tools, including:
- Wood’s lamp examination: A special type of light that helps reveal the depth of pigmentation whether it sits on the surface (epidermal), deeper in the skin (dermal), or both.
- Dermatoscopic evaluation: A magnified view of the skin using a dermatoscope to assess patterns, borders, and pigmentation characteristics that are not visible to the naked eye.
- Detailed medical and lifestyle history: Understanding hormonal influences, medication use, sun exposure, previous skin injuries, and family history can all help in identifying the root cause of the discolouration.
An accurate diagnosis ensures that the treatment plan is safe, effective, and personalised to your skin’s specific needs. It also helps prevent common setbacks like prolonged healing, increased pigmentation, or unnecessary treatments that might not work for your particular condition.
Treatment Options Compared
Treating pigmentation effectively requires knowing exactly what kind you’re dealing with, as melasma and other types of hyperpigmentation often respond very differently to treatment.
For Melasma: A Gentle, Long-Term Approach
Melasma tends to be stubborn and sensitive, so treatments must be selected and applied with care. The goal is to reduce pigmentation without triggering inflammation or worsening the condition.
- Prescription creams: Dermatologists often prescribe topical treatments containing hydroquinone (a melanin-suppressing agent), tretinoin (a vitamin A derivative that boosts skin renewal), and azelaic acid (which helps reduce pigment without causing irritation). These are sometimes used in combination for enhanced effect.
- Chemical peels: While these can be useful, they must be performed cautiously. Mild peels, such as those with mandelic or lactic acid, may help exfoliate surface pigment. However, stronger peels can cause irritation and trigger rebound pigmentation, making professional supervision essential.
- Laser therapy: Only low-energy lasers, such as Q-switched or fractional lasers, are used for melasma and even then, with caution. Aggressive laser treatments can backfire and cause worsening of pigmentation.
- Daily sun protection: This is non-negotiable. Broad-spectrum SPF 50+ sunscreen must be applied every single day, even in winter or when indoors, as UV and visible light can both aggravate melasma.
- Hormonal review: If hormonal triggers are suspected such as from birth control pills or HRT a review with a healthcare provider may help determine if adjusting medications could reduce flare-ups.
For Other Types of Hyperpigmentation: More Flexible Treatment
Post-inflammatory hyperpigmentation, sunspots, and other non-hormonal pigmentation issues usually respond more quickly to treatments and offer a wider range of options.
- Topical retinoids: These vitamin A derivatives help increase skin cell turnover, fade dark spots, and even out skin tone over time.
- Vitamin C serums: A popular antioxidant in skincare, vitamin C helps brighten the skin, reduce melanin formation, and protect against further sun damage.
- Chemical peels: Superficial to medium-depth peels containing glycolic acid, salicylicacid, or trichloroacetic acid (TCA) can be highly effective for fading dark marks. These work by exfoliating pigmented skin cells and encouraging new cell growth.
- Microneedling: This treatment involves creating tiny punctures in the skin to stimulate collagen and promote healing. When combined with pigment-reducing serums, it can improve tone and texture.
- Targeted laser therapy: Pigmentation caused by sun damage or PIH often responds well to intense pulsed light (IPL) or fractional lasers, which target pigment more directly and precisely than those used for melasma.
Note: Regardless of the type, all pigmentation treatments should be supervised by a dermatologist. Using strong actives or procedures without guidance can lead to complications such as post-inflammatory hyperpigmentation (PIH) especially in darker skin tones or worsen underlying melasma. A tailored plan based on your skin type, history, and pigmentation pattern is always the safest and most effective route.
For Other Types of Hyperpigmentation:

Unlike melasma, which often requires a slow and cautious approach, other forms of hyperpigmentation such as post-inflammatory hyperpigmentation (PIH), sunspots, or age spots generally respond more quickly and predictably to treatment. These pigment concerns often result from visible skin trauma, acne, or prolonged sun exposure, and the damage tends to be more superficial.
Here are some of the most effective options used by dermatologists:
- Topical retinoids: These vitamin A derivatives (such as tretinoin or adapalene) are widely used to treat pigmentation caused by acne or sun damage. They work by accelerating skin cell turnover, helping to shed pigmented cells more quickly and reveal a more even-toned complexion over time.
- Vitamin C serums: Vitamin C is a powerful antioxidant that not only brightens the skin but also inhibits melanin production. Regular use can reduce the appearance of dark spots while protecting the skin from free radical damage and environmental stressors.
- Chemical peels: Dermatologist-administered peels containing ingredients like glycolic acid, salicylic acid, or trichloroacetic acid (TCA) can effectively target surface-level pigmentation. These treatments exfoliate the upper layers of skin and stimulate new, healthy skin to grow in its place. Results are often noticeable after a few sessions.
- Microneedling: This minimally invasive procedure involves the use of fine needles to create micro-injuries in the skin. These tiny channels stimulate collagen production and allow pigment-fading ingredients to penetrate more deeply. When combined with brightening serums, microneedling can significantly improve skin tone and texture.
- Targeted laser therapy: For stubborn spots or deep pigmentation, dermatologists may recommend laser treatments such as Q-switched lasers or IPL (intense pulsed light). These therapies work by breaking down excess melanin in the skin so the body can naturally remove it. The key is using the right device for your skin type and pigmentation depth.
Note: No matter the type of pigmentation, it’s essential to work with a qualified dermatologist. Even seemingly mild treatments like chemical peels or retinoids can lead to post-inflammatory hyperpigmentation (PIH), especially in medium to darker skin tones. And if there’s even a chance the pigmentation is melasma, aggressive treatment could make things worse. A personalised plan based on skin tone, history, and root cause offers the safest path to real results.
Lifestyle Tips to Prevent Worsening
When managing pigmentation whether it’s melasma or another type your daily habits play a huge role in either supporting treatment or unintentionally making things worse. Even the best skincare routine won’t deliver results if external triggers are constantly reactivating melanin production. That’s why prevention is just as important as active treatment.
Here are some dermatologist-approved lifestyle adjustments to help prevent pigmentation from worsening:
- Use daily sun protection, even indoors or in winter: UV rays are one of the most powerful triggers for pigmentation. What many people don’t realise is that UVA rays can penetrate glass, meaning your skin is still exposed while sitting near a window or driving. Additionally, visible light including blue light from screens can worsen melasma in some individuals. Use a broad-spectrum SPF 50+ sunscreen every day, year-round, and reapply every 2–3 hours if you’re outside.
- Avoid excessive heat, including saunas or hot yoga: Heat can stimulate pigment-producing cells (melanocytes), even without sun exposure. Activities like hot yoga, steam rooms, or prolonged exposure to a hot kitchen can trigger or worsen melasma. Stick to cooler environments whenever possible and allow your skin to breathe.
- Be gentle with your skin no harsh scrubs or DIY peels: Over-exfoliating or using aggressive treatments at home can irritate your skin and increase inflammation, especially if you’re dealing with post-inflammatory hyperpigmentation or melasma. Skip gritty scrubs, harsh brushes, or untested online “remedies,” and focus on soothing, barrier-supportive skincare.
- Consider hormonal reviews if you suspect a trigger: If you notice your pigmentation fluctuates with your menstrual cycle, pregnancy, or after starting hormonal birth control or HRT, hormonal imbalances may be contributing. In such cases, working with a GP or endocrinologist to assess your hormone levels could support your dermatologist’s efforts in managing melasma or hormonally driven pigmentation.
Final Thought: Why a Proper Diagnosis Matters for Pigmentation Issues
Understanding the difference between melasma and general hyperpigmentation can change the course of your treatment entirely. If your pigmentation isn’t improving or seems to flare with hormonal changes don’t wait. You can get in touch with us if you’re considering private melasma treatment in London for a professional diagnosis and a personalised treatment plan.
References:
- Andersen, K.E., Davis, E.C. and Callender, V.D., 2022. A clinical review of melasma: diagnosis, pathogenesis, and management options. Journal of Clinical and Aesthetic Dermatology, 15(6), pp.38–48. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9302505/
- Sarkar, R., Bansal, A. and Garg, V.K., 2012. Chemical peels for melasma in dark-skinned patients. Journal of Cutaneous and Aesthetic Surgery, 5(4), pp.247–253. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3673383/
- Rodriguez, C.I. and Draelos, Z.D., 2017. Management of postinflammatory hyperpigmentation: a review of the literature and the role of topical agents, chemical peels, and lasers. Journal of Clinical and Aesthetic Dermatology, 10(1), pp.17–23. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5242194/
- DermNet NZ, 2022. Melasma. DermNet. Available at: https://dermnetnz.org/topics/melasma
- Passeron, T., Picardo, M., Ortonne, J.P. and Ball, A., 2019. New insight in skin depigmentation: Mechanism of action of current and emerging agents. Pigment Cell & Melanoma Research, 32(3), pp.326–345. DOI: https://doi.org/10.1111/pcmr.12738
