When you first notice a scaly, discoloured patch of skin that doesn’t clear upeven after weeks of moisturising or over-the-counter creamsit’s easy to assume it must be something common like eczema, psoriasis, or even a fungal infection. But sometimes, these stubborn patches turn out to be something less familiar: parapsoriasis.
Parapsoriasis is a rare and often misunderstood group of skin disorders that can resemble more familiar inflammatory conditions but behave quite differently beneath the surface. Unlike psoriasis or eczema, parapsoriasis may not always cause discomfort or itching, which can make it easy to ignore. However, it’s important to know that these chronic patches aren’t just a cosmetic concern. In some cases, parapsoriasis can persist for years and, more rarely, evolve into more serious conditions if left unmonitored.
Because of its subtle symptoms and visual similarity to other skin issues, parapsoriasis often goes undiagnosed or misdiagnosed. That’s why awareness and early specialist assessment are key. The sooner it’s correctly identified, the sooner you can receive appropriate careand possibly avoid complications down the line.
In this article, we’ll take a closer look at what parapsoriasis is, explore the different types, understand what causes it, and explain why regular follow-up with a dermatologist is so important. Whether you’re newly diagnosed or just curious about those lingering patches on your skin, this guide will give you the clarity and confidence to take the next step in managing your skin health.
What Is Parapsoriasis?
Parapsoriasis is a chronic inflammatory skin condition that leads to persistent, scaly, and discoloured patches or plaques on the skin. Although its name closely resembles psoriasis, and the two conditions share some visual similarities, parapsoriasis is a distinct disorder with a different clinical course and prognosis.
It is classified within the broader group of chronic inflammatory dermatosesconditions that affect the skin over time due to immune system activity. One of the key features of parapsoriasis is its slow progression and relatively subtle symptoms, which can make it difficult to detect without specialist input.
There are two main types: small plaque parapsoriasis and large plaque parapsoriasis, each varying in size, appearance, and long-term risk (more on this below).
In some casesparticularly with large plaque parapsoriasisthe condition may carry a small but important risk of evolving into cutaneous T-cell lymphoma (CTCL). CTCL is a rare form of skin cancer that affects the T-cells, a type of white blood cell that helps regulate immune responses in the skin.
While this potential progression can sound worrying, it’s important to note that:
- Most cases of parapsoriasis remain stable over time
- The majority are non-cancerous and manageable with proper dermatological care
- Regular monitoring and early diagnosis allow for timely treatment and reassurance
In many cases, people live for years with parapsoriasis without it significantly affecting their quality of life. With support from a dermatologist, flare-ups can often be controlled, and any signs of progression can be caught early.
What Does Parapsoriasis Look Like?

Parapsoriasis can be deceptively difficult to recognise. It often resembles other chronic skin conditions, which is why a proper diagnosis typically requires the trained eye of a dermatologist. At first glance, peopleand sometimes even non-specialist healthcare providersmay confuse it with eczema, psoriasis, pityriasis rosea, or even fungal infections, as it tends to appear in similar locations like the trunk, arms, thighs, or flanks.
Despite its name, parapsoriasis doesn’t always look like classic psoriasis. It’s usually milder in appearance, which can delay diagnosis or lead to assumptions that it’s nothing serious. However, these subtle presentations are exactly why professional evaluation is so crucialespecially if standard treatments aren’t working.
Common Features of Parapsoriasis:
- Flat or slightly raised patches of dry, scaly skin
- Discolouration that can appear pink, brown, yellowish, or even greyish over time
- A dry or rough texture, sometimes resembling sandpaper
- Minimal or no itchingthough a few people may notice mild discomfort or sensitivity
- Persistent lesions that remain unchanged for months or even years, with little or no response to common creams or moisturisers
These patches may come and go very slowly or remain entirely static for long periods. Unlike psoriasis, which often causes thick, silver-scaled plaques that build up quickly, parapsoriasis is generally more subtle, less inflamed, and slower to evolve.
Because of its slow progression and relatively mild symptoms, many people dismiss it as harmless or cosmetic. But identifying parapsoriasis earlyparticularly the large plaque variantcan make a big difference in long-term outcomes.
If you’ve noticed patches of skin that don’t fade, shift in colour or size, or simply haven’t improved with over-the-counter products, it’s best to consult a dermatologist. Early evaluation can lead to faster relief and provide peace of mind.
The Two Main Types of Parapsoriasis
Parapsoriasis is broadly divided into two types, based on the size, appearance, and potential behaviour of the affected skin patches: small plaque parapsoriasis and large plaque parapsoriasis. While both forms can appear similar initiallyoften showing as flat, discoloured patchestheir clinical significance and long-term risks differ quite a bit.
Understanding which type you have is crucial, as it directly influences the treatment plan and how closely your skin should be monitored over time.
1. Small Plaque Parapsoriasis
Description:
- Patches are generally smaller than 5 cm in diameter
- Most commonly found on the trunk, hips, and upper limbs
- The colour may vary, appearing pink, yellowish, or light brown, and the surface often feels slightly rough or dry
Prognosis:
- Typically regarded as benign and stable
- Carries a very low risk of progressing to cutaneous T-cell lymphoma
- In many cases, the patches remain unchanged for years and may even improve with treatment or spontaneously
Because of its low-risk nature, small plaque parapsoriasis is usually managed with topical treatments and routine follow-ups, without the need for aggressive interventions.
2. Large Plaque Parapsoriasis
Description:
- Patches are larger than 5 cm and may grow slowly over time
- These lesions can affect larger sections of the torso, thighs, or upper arms
- May display more prominent scaling, dull redness, or even signs of skin thinning (atrophy), which can feel delicate or fragile to the touch
Prognosis:
- Requires careful and regular monitoring due to a higher risk of progression
- Approximately 10–30% of large plaque cases may evolve into early-stage cutaneous T-cell lymphoma (CTCL) over several years
- Ongoing skin checks, photographic comparisons, and occasional biopsies are often recommended to detect any signs of transformation as early as possible
Why Early Diagnosis and Monitoring Matter
When it comes to parapsoriasis, especially the large plaque variant, early diagnosis isn’t just helpfulit’s essential. While most cases of parapsoriasis are benign and remain stable over time, large plaque types carry a higher risk of slowly progressing into cutaneous T-cell lymphoma (CTCL), a rare but serious skin lymphoma. This potential for transformation is why dermatologists place such strong emphasis on early detection and regular monitoring.
Catching the condition in its early stages allows specialists to establish a clear baseline, identify any patterns of change, and act quickly if anything concerning develops. Even in small plaque parapsoriasis, where the likelihood of progression is extremely low, ongoing observation helps ensure that nothing is missed.
Routine check-ups also offer patients something equally valuable: peace of mind.
Key Benefits of Early Diagnosis and Monitoring:
- Early intervention if signs of progression appear
Any suspicious changes can be addressed promptly, improving outcomes and reducing anxiety. - Clear documentation of your baseline skin condition
Knowing what your skin looked like at the start helps track even the smallest shifts over time. - Reassurance through regular expert follow-up
Staying connected with your dermatologist means you’re not navigating uncertainty aloneand that support can make a big difference in how you manage your condition.
Ultimately, whether your parapsoriasis remains unchanged for years or starts to show signs of progression, being under the care of a skin specialist gives you a head start. With expert guidance, you can feel confident that your skin health is being carefully and proactively managed.
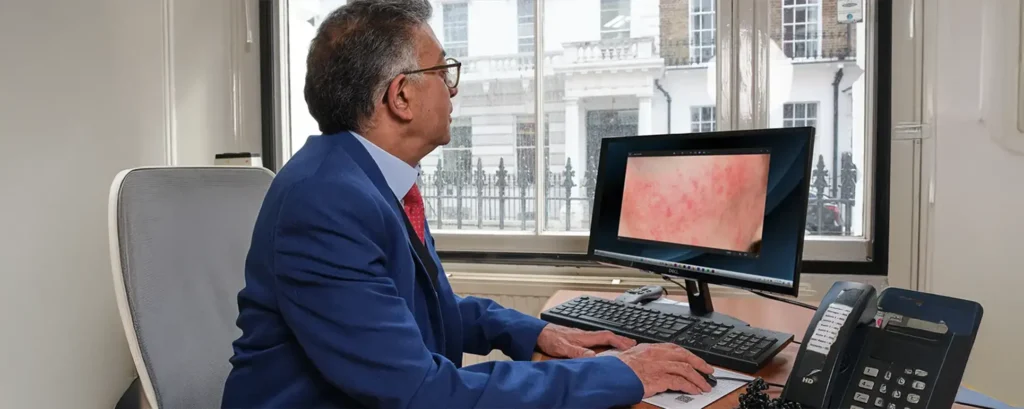
How Dermatologists Diagnose Parapsoriasis
Diagnosing parapsoriasis is not always straightforward. The condition can look deceptively similar to other chronic skin issueslike eczema, psoriasis, or fungal infectionswhich is why a detailed evaluation by a dermatologist is essential. Diagnosis typically involves a combination of clinical observation, discussion of your medical history, and occasionally, laboratory testing to rule out other possibilities or confirm subtle changes.
Here’s what you can usually expect during a dermatology consultation:
- Visual Assessment:
Your dermatologist will carefully inspect the affected areas, noting the size, shape, colour, texture, and distribution of the patches. While many skin conditions can look similar on the surface, experienced specialists are trained to identify the subtle features that may point towards parapsoriasis. - Medical History:
You’ll be asked about when the patches first appeared, how they’ve behaved over time, and whether you’ve tried any treatments. Information about personal or family history of skin conditions, immune-related disorders, or past biopsies also helps shape the diagnostic process. - Skin Biopsy:
If there’s uncertainty or the presentation suggests large plaque parapsoriasis, your dermatologist may perform a biopsy. This involves removing a small sample of skin under local anaesthetic for microscopic examination. The biopsy helps differentiate parapsoriasis from similar-looking conditions and may also reveal early signs of cutaneous T-cell lymphoma (CTCL), if present. - Photographic Documentation:
High-quality clinical photos are often taken to create a visual record. These images are extremely useful for tracking changes over timeespecially if the condition is stable or evolving slowly.
By combining all these steps, dermatologists can make a confident diagnosis and recommend an appropriate treatment and monitoring plan. Early and accurate identification ensures you get the right care, and helps prevent unnecessary treatments or delays in managing more serious conditions if they arise.
Treatment Options for Parapsoriasis

Topical treatments are often the first step in managing parapsoriasis, especially when the affected areas are limited or the condition is mild. These therapies aim to soothe the skin, reduce inflammation, and improve the appearance of patches.
- Corticosteroid Creams:
These are commonly prescribed anti-inflammatory medications that help reduce redness, scaling, and irritation. They’re usually applied once or twice daily to affected areas and can lead to noticeable improvement with consistent use. - Emollients (Moisturisers):
Hydration is key in managing chronic skin conditions. Emollients help lock in moisture, soften rough patches, and minimise flaking. They can be used daily alongside other treatments to maintain skin health. - Topical Retinoids:
Occasionally, dermatologists may prescribe retinoid creams (vitamin A derivatives) to help regulate skin cell turnover. These are more commonly used in stubborn cases or when patches show signs of abnormal cellular behaviour.
Phototherapy
When topical treatments aren’t enough, or if the condition is more widespread, light therapyalso known as phototherapymay be recommended. This involves exposing the skin to specific wavelengths of ultraviolet light under medical supervision.
- Narrowband UVB Therapy:
This is a widely used option that delivers targeted UVB light to affected areas, helping to slow abnormal skin cell growth and reduce inflammation. It’s considered safe for long-term use and doesn’t carry significant systemic risks. - PUVA Therapy (Psoralen + UVA):
PUVA involves taking a medication called psoralenwhich makes the skin more sensitive to lightbefore being exposed to UVA light. It’s typically reserved for more resistant or extensive cases and requires careful monitoring due to potential side effects.
Phototherapy is generally carried out in a clinical setting and may require multiple sessions over several weeks to see results. Maintenance therapy may also be considered in some cases.
Ongoing Monitoring
Regular monitoring is a crucial part of managing parapsoriasis, especially in cases of large plaque parapsoriasis, where there’s a slightly elevated risk of progression to cutaneous T-cell lymphoma (CTCL). The goal is to catch any changes early so that treatment can be adjusted promptly.
- Routine Follow-Ups:
Dermatologists usually recommend check-ups every 3 to 12 months, depending on how stable the condition is. During these visits, the skin is examined closely for any signs of thickening, colour changes, or new lesions. - Repeat Biopsies:
If any patch starts to look suspiciousbecoming firmer, darker, or more irregular in shapea new biopsy may be recommended. This helps rule out lymphoma or other evolving skin conditions.
Consistent monitoring allows for peace of mind and ensures that any potential concerns are addressed early, before they become more serious.
Reassurance for Patients
Being told that your skin condition needs to be monitored for cancer risk can understandably be unsettling. However, it’s important to keep things in perspective.
- The vast majority of parapsoriasis casesparticularly small plaqueremain stable and never progress to lymphoma.
- Regular reviews are simply a precautionary measure to ensure that any early changes are caught before they pose a risk.
- Even if CTCL does develop, early detection gives you the best chance at successful treatment. Today’s therapies are much more effective than in the past and often allow people to manage the condition well.
Remember, seeing your dermatologist regularly is not about expecting the worstit’s about being prepared, informed, and supported.
When Should You See a Dermatologist?
If you’ve noticed any skin patches that don’t seem to be improvingor are slowly getting worseit’s worth booking a specialist consultation. In particular, you should seek expert advice if the patches:
- Have lasted for more than six months without significant change
- Are gradually increasing in size or spreading to new areas
- Haven’t responded to treatments like steroid creams, moisturisers, or antifungal creams
- Are showing changes in texture, such as becoming thinner, thicker, or more wrinkled
Early diagnosis helps distinguish between benign skin conditions and those that require closer follow-up or treatment. Getting clarity sooner rather than later is always the best option.
Tips for Living with Parapsoriasis
Living with a chronic skin condition like parapsoriasis can be challenging, but small daily habits can go a long way in managing your symptoms and protecting your skin.
- Keep a photo diary:
Take clear photos of your patches every few weeks. This helps you and your dermatologist track any changes over time. - Use emollients daily:
Moisturising regularly strengthens your skin barrier, soothes dryness, and reduces flaking. - Wear soft, breathable clothing:
Loose, cotton-based fabrics reduce friction and irritation, especially in sensitive areas. - Be cautious with sun exposure:
While some UV light may help, excessive sun can damage the skin or worsen symptoms. Follow your doctor’s advice about sun protection or light therapy. - Don’t skip follow-up appointments:
Even if your skin looks stable, routine reviews are essential. They allow your dermatologist to catch any subtle changes you might not notice.
With consistency and medical support, most people with parapsoriasis can lead full, comfortable lives while keeping the condition under control.
Final Thought: When to Seek Clarity for Patchy Skin Changes
Parapsoriasis is a lesser-known condition, but it’s more common than many realise. With proper evaluation, monitoring, and treatment, most people can live comfortably without complications. If you’re dealing with persistent patchy skin changes that haven’t improved, consider booking a consultation at our specialist psoriasis clinic in London. Early reassurance and clarity can make all the difference.
References:
- Chairatchaneeboon, M., Thanomkitti, K. & Kim, E.J., 2022. ParapsoriasisA Diagnosis with an Identity Crisis: A Narrative Review. Dermatology and Therapy, 12(5), pp.1091–1102. doi:10.1007/s13555-022-00716-y. Available at: https://doi.org/10.1007/s13555-022-00716-y
- Väkevä, L., Sarna, S., Vaalasti, A., Pukkala, E., Kariniemi, A-L. & Ranki, A., 2005. A retrospective study of the probability of the evolution of parapsoriasis en plaques into mycosis fungoides. Acta Dermato‑Venereologica, 85(4), pp.318–323. doi:10.1080/00015550510030087. Available at: https://pubmed.ncbi.nlm.nih.gov/16191852
- Duarte, I.A.G., Korkes, K.L. & Amorim, V.A., 2013. An evaluation of the treatment of parapsoriasis with phototherapy. Anais Brasileiros de Dermatologia, 88(2), pp. 306–308. doi:10.1590/S0365-05962013000200028. Available at: https://pubmed.ncbi.nlm.nih.gov/23739710/Medscape, 2025. Parapsoriasis: Background, Pathophysiology, Epidemiology. eMedicine Dermatology. Available at: https://emedicine.medscape.com/article/1107425-overview
- DermNet NZ, 2023. Chronic Superficial Scaly Dermatitis (Parapsoriasis). Available at: https://dermnetnz.org/topics/chronic-superficial-scaly-dermatitis
