Scar treatment has evolved significantly over the past decade. Where options were once limited to surgery or resurfacing, regenerative medicine has opened the door to treatments that aim to heal skin from within. You’ve likely heard about PRP, growth factors, and even stem-cell–based therapies being promoted as next-generation solutions for scars.
If you’re considering these treatments, it’s natural to wonder whether the science matches hype. These approaches promise improved texture, better healing, and more natural results, but they also come with higher costs and varying levels of evidence. Understanding what they can and cannot do is essential before committing.
In this article, I’ll walk you through how PRP and stem-cell–based scar treatments work, what results are realistic, how they’re best combined with other procedures, and whether they truly offer value as part of a modern scar-revision plan heading into 2026.
Why Scar Treatment Is Moving Toward Regeneration
Traditional scar treatments often focus on removing damaged tissue or resurfacing the skin. While effective, these methods don’t always address the underlying biological issue, which is incomplete or disorganised healing at a cellular level.
Regenerative treatments aim to stimulate your skin’s natural repair processes. Instead of forcing change from the outside, they encourage collagen remodelling, improved blood supply, and healthier tissue formation from within.
This shift toward regeneration is why PRP and stem-cell–based treatments have gained attention. They are designed to enhance healing rather than simply mask or abrade scars.
Understanding PRP in Scar Treatment

Platelet-rich plasma, commonly known as PRP, is derived from your own blood. A small blood sample is taken and spun in a centrifuge to separate platelets from other components.
These platelets are rich in growth factors, which play a critical role in wound healing and tissue repair. When injected into scarred skin, PRP releases these growth factors gradually, encouraging collagen production and improved tissue quality. Because PRP uses your own blood, it is considered autologous, meaning the risk of allergic reaction is extremely low.
How PRP Improves Scar Appearance
PRP does not fill scars or remove them instantly. Instead, it works over time by improving the skin’s biological environment. Growth factors released by platelets stimulate fibroblasts, the cells responsible for collagen production.
As collagen remodels, the scar may become smoother, softer, and less noticeable. Blood flow to the area can also improve, supporting healthier skin tone and texture. Results are gradual and typically develop over several weeks to months, which is important to understand before starting treatment.
Types of Scars That Respond Best to PRP
PRP is most effective for scars where texture and tissue quality are the main concerns. This includes mild to moderate acne scars, early surgical scars, and injury-related scars that have healed but remain uneven.
Deep, tethered scars often require additional treatments such as subcision or fillers before PRP can be effective. Raised scars like keloids do not typically respond well to PRP alone. Your dermatologist will assess whether PRP is suitable for your scar type during consultation.
What Are Growth-Factor-Based Treatments?
Growth-factor therapy refers to topical or injectable products that contain laboratory-derived growth factors. These are often used alongside microneedling or laser treatments to enhance healing.
Unlike PRP, which uses your own platelets, growth-factor products are manufactured under controlled conditions. They aim to deliver consistent concentrations of specific signalling proteins to the skin.
These treatments can support skin repair, but their effectiveness depends heavily on formulation quality and how they are delivered.
Stem-Cell–Based Treatments Explained
Stem-cell–based treatments are often surrounded by confusion and misconceptions. Many people assume that these procedures involve injecting live stem cells directly into the skin, but in most aesthetic and dermatology clinics, this is not the case.
Instead, these treatments typically use derivatives of stem cells, such as conditioned media or exosomes. These substances are rich in signalling molecules that stem cells naturally release, which play a key role in communication between cells and tissue repair.
The signalling molecules in these products help stimulate healing, collagen production, and regeneration in the skin. By influencing the skin’s natural repair processes, they can improve texture, tone, and overall skin quality over time.
The main advantage of using stem-cell derivatives is that they provide the benefits of stem-cell signaling without the risks associated with transplanting live stem cells, such as immune reactions or complications from cell integration.
How Stem-Cell–Derived Products Work on Scars
Stem-cell–derived products work by releasing a variety of bioactive molecules that play an important role in the skin’s healing processes. These molecules can influence inflammation, stimulate collagen production, and support tissue remodelling, all of which are critical for improving the appearance of scarred skin. By creating a more favourable environment for skin repair, these treatments can help the tissue recover in a smoother, more balanced way over time.
When applied or injected into scarred areas, stem-cell derivatives are often combined with other procedures such as microneedling or laser therapy. These additional treatments enhance the penetration and effectiveness of the bioactive molecules, allowing them to reach deeper layers of the skin where they can have a greater impact.
It is important to note that while stem-cell–derived products can improve skin quality and support healing, they are unlikely to dramatically change deep or severe scars when used alone. Research in this field is still ongoing, and although early results are promising, individual outcomes may vary depending on scar type, skin condition, and the specific treatment protocol used.
The Science: What Evidence Supports These Treatments?
Regenerative treatments for scars vary in scientific support, with some backed by robust studies while others are still emerging. Evidence helps guide both dermatologists and patients in choosing the most effective approaches. Understanding the research behind each option can clarify expected outcomes and set realistic expectations.
- PRP (Platelet-Rich Plasma) has the strongest scientific backing, showing consistent improvements in acne scar texture when combined with microneedling or laser therapy.
- Growth-factor treatments have moderate evidence, mainly supporting faster healing and reduced downtime, though their standalone impact on scars is less established.
- Stem-cell–based products show promising potential in laboratory and early clinical studies, but long-term and large-scale trial data remain limited.
- Overall, combining these treatments with other modalities often maximizes results and provides more comprehensive scar improvement.
Realistic Results You Can Expect
Regenerative treatments, including PRP and stem-cell–based therapies, should not be considered miracle cures for scars. Their primary benefit lies in improving overall skin quality, texture, and tone rather than completely erasing the appearance of scars.
With PRP (platelet-rich plasma) therapy, many individuals notice smoother skin texture, softer and less defined scar edges, and a more even skin tone. These changes develop gradually over several weeks, and achieving noticeable results typically requires multiple treatment sessions spaced appropriately by your clinician.
Setting realistic expectations before starting any regenerative treatment is crucial. Understanding the limitations of these therapies helps patients avoid disappointment and ensures they are satisfied with the gradual, natural improvements that are achievable over time.
Why Combination Treatments Matter
Scars are complex and involve multiple layers of skin, so a single treatment rarely addresses every aspect of their appearance. Combining therapies allows each modality to target specific scar characteristics, leading to more effective and balanced results. Treatments that stimulate healing work best when paired with agents that enhance tissue regeneration, maximizing overall improvement.
- PRP is most effective when combined with procedures like microneedling, laser resurfacing, or subcision, which create controlled skin injury to stimulate healing.
- These procedures trigger the skin’s natural repair mechanisms, while PRP enhances collagen production and accelerates recovery.
- Stem-cell–derived products show better results when paired with treatments that open channels in the skin, allowing for deeper penetration and more pronounced effects.
- Overall, combination treatments provide a synergistic approach, addressing texture, volume, and skin quality simultaneously for optimal scar improvement.
PRP with Microneedling for Scars
Microneedling works by creating controlled micro-injuries in the skin, which triggers the body’s natural healing response and stimulates collagen and elastin production. When combined with PRP (platelet-rich plasma), the healing process is further enhanced, as the growth factors in PRP accelerate tissue repair and regeneration.
The results of PRP with microneedling are generally more noticeable than microneedling alone, as the added growth factors help the skin remodel more efficiently. For optimal outcomes, multiple treatment sessions are usually recommended, spaced several weeks apart, allowing gradual and cumulative improvement in both skin texture and scar appearance.
Stem-Cell Treatments as Adjuncts, Not Replacements
Stem-cell–based products are best understood as supportive therapies rather than standalone solutions for scar revision. While they can enhance healing, stimulate collagen, and improve overall skin quality, they rarely replace established and proven procedures such as fillers, microneedling, or laser treatments.
When incorporated into a comprehensive, structured scar-revision plan, stem-cell–derived treatments can add significant value. They are particularly useful for patients looking for gradual, incremental improvements in skin texture and appearance rather than dramatic, immediate results.
Working with a reputable scar treatment clinic in London ensures that these therapies are administered safely, effectively, and ethically. Experienced specialists can determine the appropriate role of stem-cell treatments within a broader plan, combining them with other modalities for the most balanced and natural outcomes.
How Many Sessions Are Typically Needed
PRP treatments for scars generally require a series of three to four sessions, with each session spaced several weeks apart to allow the skin to heal and respond fully. The number of sessions may vary depending on the severity of the scars, individual skin response, and the goals of treatment. Some patients may also benefit from periodic maintenance sessions to sustain and enhance the results over time.
Similarly, growth-factor and stem-cell–derived treatments often follow comparable schedules, especially when used in combination with other procedures such as microneedling or laser therapy. Because the improvements from these regenerative therapies are gradual and cumulative, patience and consistency are key to achieving the best possible outcomes.
Safety Considerations You Should Know
PRP is generally considered very safe because it is autologous, meaning it is prepared from your own blood. As a result, the risk of allergic reaction is extremely low, with side effects usually limited to temporary swelling, redness, tenderness, or mild bruising at the injection sites.
Growth-factor products are also typically well tolerated when they are sourced from reputable, regulated manufacturers. However, quality and processing standards vary, which is why product selection and clinical expertise play a crucial role in safety and outcomes.
Stem-cell–derived treatments can differ significantly in both quality and regulatory oversight. Because of this variability, it is especially important to choose an experienced, medically led clinic that follows strict safety protocols and provides clear guidance on what is being used and why.
Cost vs Value: Are These Treatments Worth It?
Regenerative treatments are often more expensive than traditional scar therapies, largely because they rely on advanced techniques and biological processes. Whether they are worth the investment depends on your individual goals, the type and severity of your scars, and your willingness to commit to multiple treatment sessions over time.
For mild to moderate scars, PRP combined with microneedling can offer good value by improving skin texture and tone with minimal downtime. Many patients find this approach appealing because it delivers gradual, natural-looking improvements without significantly disrupting daily life.
Stem-cell–based treatments may be worth considering as part of a broader, long-term treatment plan, particularly for more complex scarring. However, they are rarely cost-effective as standalone solutions and tend to work best when combined with other proven therapies under expert guidance.
Who Is an Ideal Candidate?
Ideal candidates for regenerative scar treatments typically have scars that are stable, fully healed, and mainly textural in nature. Overall good health and realistic expectations are important for achieving satisfying results. Certain skin conditions or active issues need to be managed before starting treatment to ensure safety and effectiveness.
- Candidates should have scars that are mature and stable, with minimal active inflammation or ongoing acne.
- Good general health supports healing and reduces the risk of complications during and after treatment.
- Dermatologists will assess each patient’s suitability carefully, considering skin type, scar characteristics, and treatment goals.
- Not every patient requires regenerative treatments, and a personalized plan ensures honest guidance and optimal outcomes.
How These Treatments Fit Into a 2026 Scar-Revision Plan
Looking ahead, scar treatment is becoming increasingly personalised. Rather than relying on one method, modern plans combine resurfacing, mechanical release, volume restoration, and regeneration.
PRP is likely to remain a core regenerative option due to its safety and evidence base. Stem-cell–derived therapies may continue to evolve as research advances. The key is integration rather than replacement of proven treatments.
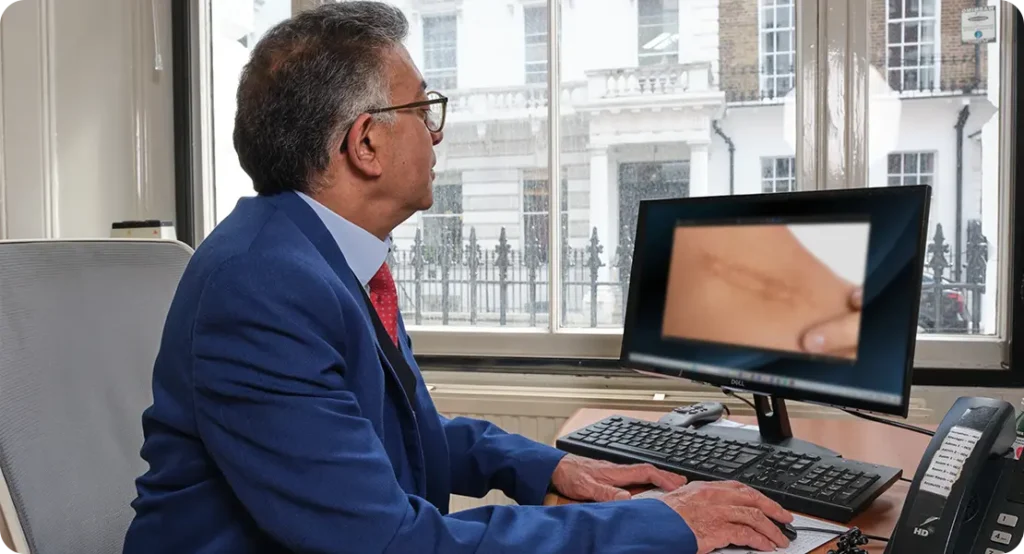
Choosing the Right Clinic Makes the Difference
Regenerative scar treatments rely on clinical expertise, not just advanced equipment. Careful assessment, precise technique, and thoughtful combination planning all play a crucial role in achieving meaningful, lasting results.
A dedicated scar treatment clinic in London provides a comprehensive evaluation and evidence-based treatment pathway, rather than offering trend-driven or one-size-fits-all solutions. This approach helps ensure that your time, effort, and investment lead to genuine, visible improvement.
FAQs:
1. What is PRP and how does it help with scar treatment?
Platelet-rich plasma, or PRP, is a treatment derived from your own blood, which is processed to concentrate platelets rich in growth factors. When injected into scarred skin, these growth factors gradually stimulate collagen production and improve tissue quality. PRP works by enhancing the skin’s natural healing processes rather than instantly removing scars, leading to gradual improvements in texture, softness, and overall skin tone over several weeks or months.
2. How do stem-cell–based treatments work for scars?
Stem-cell–based treatments typically use derivatives of stem cells, such as exosomes or conditioned media, rather than live stem cells. These derivatives contain signalling molecules that influence cellular communication and tissue repair. When applied or injected into scarred areas, they promote collagen production, modulate inflammation, and support tissue remodelling. Over time, this can improve the skin’s texture, tone, and resilience, though they are unlikely to dramatically change deep or severe scars when used alone.
3. Are PRP and stem-cell treatments suitable for all types of scars?
These regenerative treatments are most effective for scars that primarily involve texture and tissue quality, such as mild to moderate acne scars, early surgical scars, and healed injury scars. Deep, tethered scars often require additional interventions such as subcision or fillers, and raised scars like keloids do not typically respond well to PRP or stem-cell therapies alone. A dermatologist will assess scar type, depth, and stability to determine suitability for treatment.
4. How many sessions are usually needed to see results?
Most PRP treatments involve a series of three to four sessions spaced several weeks apart, with maintenance treatments sometimes recommended. Stem-cell–derived and growth-factor-based treatments often follow a similar schedule when used alongside other procedures. Because results are cumulative and gradual, multiple sessions are typically necessary to achieve the desired improvements in texture and skin quality.
5. How quickly can I expect to see improvements after treatment?
Unlike fillers or surgical interventions that provide immediate effects, PRP and stem-cell-based treatments work gradually. Patients usually notice subtle improvements in scar texture, softness, and skin tone within several weeks, with more visible changes developing over months. The gradual nature of the results requires patience and consistent follow-up sessions to maximize the benefits.
6. Can these treatments be combined with other procedures?
Regenerative therapies often deliver the best results when combined with other treatments. PRP is frequently paired with microneedling, laser resurfacing, or subcision, which create controlled skin injury to stimulate natural healing. Stem-cell derivatives are more effective when combined with procedures that allow deeper penetration of the bioactive molecules, creating a synergistic effect that enhances collagen production, tissue regeneration, and overall skin quality.
7. Are PRP and stem-cell treatments safe?
PRP is generally very safe because it uses the patient’s own blood, and the risk of allergic reaction is extremely low. Stem-cell–derived and growth-factor products are usually well tolerated when sourced from reputable manufacturers, but the quality and regulation of these products can vary widely. Choosing an experienced clinic ensures proper technique, reduces risks, and increases the likelihood of natural, balanced results.
8. What are the realistic outcomes of regenerative scar treatments?
These treatments primarily improve skin texture, tone, and overall quality rather than erasing scars entirely. Patients often experience softer, less defined scar edges and a smoother skin surface. Dramatic changes in deep or severe scars are unlikely when using PRP or stem-cell therapies alone, so the most realistic expectations involve subtle, gradual improvements that enhance the overall appearance of the treated area over time.
9. How much do these treatments cost, and are they worth it?
Regenerative treatments are usually more expensive than traditional scar therapies because they involve advanced preparation, specialized products, and multiple sessions. Their value depends on the type and severity of scars, patient goals, and willingness to commit to ongoing treatments. For mild to moderate scars, PRP combined with other procedures can offer meaningful improvement with minimal downtime, while stem-cell-based therapies are better considered as adjuncts rather than standalone solutions.
10. Who is an ideal candidate for PRP or stem-cell scar treatments?
Ideal candidates have mature, fully healed scars that are primarily textural rather than raised or inflamed. Good overall health, realistic expectations, and commitment to multiple sessions contribute to optimal results. Patients with active acne, ongoing inflammation, or certain skin conditions may need to address these issues before starting treatment. A personalized consultation with a qualified dermatologist ensures the treatment plan matches the patient’s needs and provides the safest, most effective approach.
Final Thoughts: Regenerative Scar Treatments and What to Expect
PRP and stem cell based scar treatments represent an exciting advance in regenerative dermatology, offering gradual improvement in skin texture, tone, and overall quality. While they are not miracle cures and work best for specific scar types, they can be highly effective when integrated into a comprehensive, personalised treatment plan alongside procedures like microneedling, laser therapy, or subcision. For safe, evidence-based results, it’s important to choose an experienced provider. If you’re looking for a scar treatment clinic in London, you can book a consultation with one of our specialists at the London Dermatology Centre today to discuss the most suitable approach for your skin.
Reference
1. Brezeanu, A.‑M., Brezeanu, D., Stase, S., Chirila, S. & Tica, V.‑I. (2025) Intraoperative Platelet‑Rich Plasma Application Improves Scar Healing After Cesarean Section: A Prospective Observational Pilot Study, Healthcare, 13(22), 2905. https://www.mdpi.com/2227-9032/13/22/2905?utm_source=chatgpt.com/
2. Majewska, L., Kondraciuk, A., Dorosz, K. & Budzyńska, A. (2025) Application of Standardized Rosa damascena Stem Cell‑Derived Exosomes in Dermatological Wound Healing and Scar Management: A Retrospective Case‑Series Study with Long‑Term Outcome Assessment, Pharmaceutics, 17(7), 910. https://www.mdpi.com/1999-4923/17/7/910/
3. Alam, M. & Tredget, E.E. (2022) Platelet‑rich plasma in the treatment of scars: systematic review and meta‑analysis, Journal of Cosmetic and Laser Therapy, 24(3), pp. 123‑132. https://pubmed.ncbi.nlm.nih.gov/35795892/
4. Sclafani, A.P. & Azzi, J. (2020) Platelet‑rich plasma in noninvasive procedures for atrophic acne scars: systematic review and meta‑analysis, Dermatologic Surgery, 46(5), pp. 619‑627. https://pubmed.ncbi.nlm.nih.gov/32061047/
5. Ghobadi, F., Mohammadi, M., Kalantarzadeh, R. & Lotfi, E. (2025) Platelet‑Rich Plasma (PRP) and Recombinant Growth Factor Therapies in Wound Healing: Mechanisms, Clinical Applications, and Future Directions, Journal of Clinical Medicine, 14(23), 8583. https://www.mdpi.com/2077-0383/14/23/8583/
