Skin rashes are one of the most frequent reasons people seek medical advice. They can appear suddenly, change quickly, and vary widely in appearance from dry, scaly patches to red, itchy bumps. While many rashes are relatively harmless and go away with over-the-counter creams or simple lifestyle changes, others may be a sign of an underlying health condition that requires prompt medical attention.
But how do you know when a rash is something to keep an eye on and when it’s time to book an appointment with a dermatologist? The challenge is that rashes can look very similar on the surface, even if their causes range from allergic reactions to autoimmune diseases or infections. That’s why accurately diagnosing a rash often requires a trained eye and a thorough clinical evaluation.
In this article, we’ll explore how dermatologists evaluate skin rashes. From taking a detailed patient history and examining the appearance of the rash to ordering lab tests or biopsies when needed, you’ll get a behind-the-scenes look at how skin specialists make their assessments. We’ll also highlight warning signs that signal a rash might be more serious and explain why trying to self-diagnose through online images or home remedies can sometimes do more harm than good. Whether your rash is itchy, painful, or just mysterious, understanding the diagnostic process can help you feel more confident about what steps to take next.
First Things First: Listening to You
Before a dermatologist even looks at your skin, they start by listening closely to your story. Your medical history, symptoms, and daily habits often hold the first crucial clues to what’s really going on. Many skin conditions can look alike on the surface redness, bumps, or patches but the context behind them often tells a very different story. That’s why dermatologists place so much importance on the initial conversation.
You can expect them to ask a series of detailed questions aimed at understanding not just the rash itself, but the bigger picture of your health and lifestyle. They’ll want to know when the rash first appeared was it an abrupt onset overnight, or did it develop gradually over several days or weeks? Understanding the timeline helps rule out certain causes and focus on others.
They’ll also ask about how the rash feels:
- Is it itchy, burning, or painful?
- Does it tingle or feel numb?
- Have the symptoms changed over time?
Next, your dermatologist may dig into recent changes in your environment, habits, or routines. These could include things like:
- Switching to a new laundry detergent or skincare product
- Starting or stopping medications
- Recent travel or outdoor exposure
- Any changes in your diet or supplements
They may even ask whether you’ve been under stress, had a recent illness, or been around others with similar symptoms. This kind of thorough questioning might seem unrelated at first, but it’s a key step in ruling out or identifying possible triggers. For example, if the rash appeared shortly after starting a new medication, that clue could point toward a drug reaction. If it worsens in the sun, it might suggest photosensitivity.
Visual Inspection: Trained Eyes See More

Once your dermatologist has gathered all the details from your story, they’ll move on to the physical exam and this is where their trained eye really comes into play. While it might just look like a red patch or some bumps to you, a dermatologist sees much more than meets the eye. Years of experience and medical training allow them to detect subtle visual patterns and features that most people wouldn’t think to notice.
They assess not just the colour or size of the rash, but a full range of characteristics. This includes the shape and border of the lesions are they round, oval, irregular, or sharply demarcated? Clear borders may suggest conditions like ringworm, while more diffuse edges might indicate eczema or an allergic reaction.
Texture is another key feature. Is the skin smooth, rough, scaly, crusted, or moist? Some rashes flake or peel, while others ooze or form blisters. Each of these textures tells a different story about what’s happening beneath the skin.
Distribution is especially important. Dermatologists observe where on the body the rash appears, whether it’s confined to one area or spread across multiple regions. For instance:
- A rash that affects only sun-exposed areas may suggest a photosensitivity reaction.
- A rash in skin folds might point to a fungal infection or intertrigo.
- A symmetrical rash that appears in the same place on both sides of the body could indicate an autoimmune or systemic issue.
They’ll also evaluate whether the lesions are flat, raised, blistered, or pustular, as this detail helps differentiate between things like viral infections, inflammatory skin diseases, or allergic reactions.
Here are some of the things they might consider:
- Are the lesions grouped together or scattered?
- Is the skin dry, flaky, greasy, or weeping fluid?
- Does the rash appear only in one area or follow a specific nerve pattern?
Sometimes, what seems like a random red patch to you might actually follow a very classic and recognisable distribution. For example, a rash that wraps around one side of the torso might suggest shingles, while a butterfly-shaped rash on the face could be a sign of lupus.
Rule Out the Dangerous Stuff First
When assessing a rash, one of the top priorities for any dermatologist is to make sure it’s not a sign of something potentially life-threatening. While most rashes are harmless or easily treatable, some can be early indicators of serious systemic conditions that require immediate medical intervention. Dermatologists are trained to spot these warning signs quickly and decisively, because acting fast can make a crucial difference in outcomes.
Certain red flags immediately raise concern. For example, if a rash appears suddenly and is accompanied by fever, swollen lymph nodes, joint pain, facial swelling, difficulty breathing, or extensive blistering, it could point to a serious underlying issue. In such cases, dermatologists will act swiftly sometimes recommending hospitalisation, lab tests, or urgent referrals to other specialists.
Here are some critical conditions they aim to rule out early in the diagnostic process:
- Stevens-Johnson Syndrome (SJS) – A rare but severe reaction usually triggered by medications or infections. It causes painful blisters and peeling of the skin and mucous membranes. SJS is a medical emergency and can be fatal without prompt treatment.
- Meningococcal Septicaemia – A fast-moving bacterial infection that causes a purplish rash which doesn’t fade under pressure (a key sign). This can lead to shock, organ failure, and death if not treated immediately.
- Lupus (Systemic Lupus Erythematosus) – An autoimmune disorder that can cause a characteristic “butterfly” rash across the cheeks and nose, along with joint pain, fatigue, and organ involvement. Lupus requires long-term management and early diagnosis is vital to prevent complications.
- Erythroderma – A rare but serious condition involving widespread inflammation and scaling of the skin. It can be a reaction to medications or an exacerbation of chronic skin diseases like psoriasis. Because it affects the body’s ability to regulate temperature and retain fluids, it’s considered a dermatological emergency.
- Anaphylaxis with Urticaria (Hives) – A severe allergic reaction that may begin with hives but can quickly escalate to throat swelling, breathing difficulties, and drop in blood pressure. Recognising this early allows life-saving interventions like adrenaline injection.
Dermatologists are trained to detect when a rash is more than skin deep. If there’s any suspicion of a systemic condition, they don’t wait to take action they’ll order urgent blood tests, skin biopsies, or direct the patient to emergency care if necessary.
Patch Testing and Skin Biopsies
Sometimes, even after a detailed history and a careful visual examination, the cause of a rash isn’t immediately clear. In these cases, dermatologists turn to diagnostic tools like patch testing and skin biopsies to get definitive answers. These procedures may sound intimidating, but they’re safe, straightforward, and incredibly valuable for reaching an accurate diagnosis.
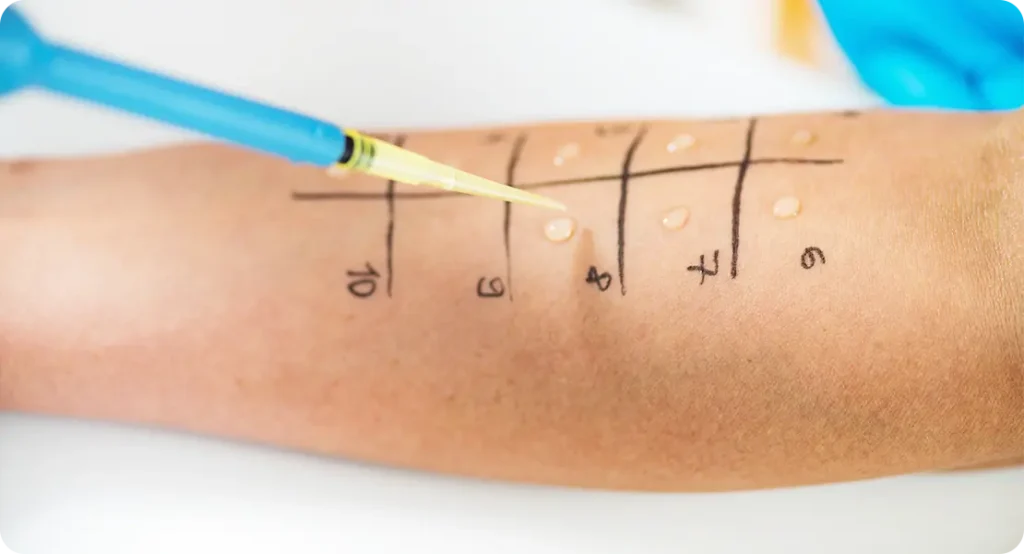
Patch Testing
Patch testing is a widely used method when an allergic reaction is suspected particularly allergic contact dermatitis, which happens when the skin reacts to something you’ve touched. This could be anything from a new soap or shampoo to metal in jewellery, or even ingredients in skincare or cleaning products.
During patch testing, small amounts of various potential allergens are placed on your back using specialised adhesive patches. You’ll wear these patches for about 48 hours, and then your dermatologist will evaluate the skin’s response at multiple intervals usually at 48 and 72 hours, and sometimes again at 96 hours. If you’re allergic to any of the substances tested, a reaction such as redness, swelling, or small blisters will appear in that specific area.
This method helps identify delayed-type allergic reactions, which may not show up immediately after exposure, making them harder to detect through history alone. Once an allergen is confirmed, you can take steps to avoid it and prevent future flare-ups.
Skin Biopsies
When a rash is persistent, unexplained, or looks unusual, your dermatologist may suggest a skin biopsy. This involves removing a small sample of the affected skin usually under local anaesthesia so it can be examined under a microscope by a dermatopathologist.
There are a few types of skin biopsies:
- Punch biopsy: A small, circular tool removes a core of skin, including deeper layers.
- Shave biopsy: A thin layer of skin is scraped off the surface.
- Excisional biopsy: A larger piece of skin is cut out, often used when there’s a need to examine the full depth or when skin cancer is suspected.
Biopsies help diagnose a wide range of skin conditions, from chronic inflammatory diseases like psoriasis, eczema, or lichen planus, to infections or even early signs of skin cancer such as basal cell carcinoma or melanoma. The results can guide the next steps whether it’s starting a treatment plan or referring to another specialist.
When It’s Probably Not Serious
The good news? Not every rash is a medical emergency. In fact, most rashes turn out to be relatively minor and manageable with the right treatment. These common skin conditions may look alarming at first, especially if they’re itchy or uncomfortable, but they usually respond well to topical creams, over-the-counter remedies, or simple changes in daily routine.
Some examples of less serious, yet still bothersome, rashes include:
- Heat Rash (Prickly Heat): Often caused by blocked sweat ducts, heat rash tends to appear in hot, humid conditions or after exercise. It usually shows up as small red bumps or clear blisters in areas where sweat gets trapped like underarms, the neck, or the back. Fortunately, this rash typically clears up on its own with cooling and loose clothing.
- Eczema (Atopic Dermatitis): A chronic skin condition that causes dry, itchy, and inflamed skin. It often flares up due to triggers like stress, allergens, soaps, or cold weather. While eczema isn’t dangerous, it can become very uncomfortable if not managed properly. Dermatologists often recommend moisturisers, steroid creams, and avoiding known irritants.
- Fungal Infections (e.g. Ringworm or Athlete’s Foot): Despite the name, ringworm isn’t caused by a worm it’s a fungal infection that forms a distinctive ring-shaped rash. Fungal rashes can appear on the scalp, feet, groin, or body, and are usually itchy and red. Antifungal creams are often effective, especially when started early.
- Mild Contact Dermatitis: This occurs when your skin comes into contact with something irritating or allergenic, such as nickel jewellery, fragranced lotions, or certain plants. The result is redness, itching, and sometimes minor swelling or flaking. Once the irritant is identified and avoided, and a topical treatment is applied, the rash often fades within days.
While these conditions are considered non-urgent, they still deserve attention. Leaving even a mild rash untreated can lead to complications like secondary bacterial infections from scratching or long-term skin thickening from chronic inflammation. In some cases, what appears to be a “simple rash” may actually mask another condition that needs a different kind of treatment.
Treatment Tailored to You

Once your dermatologist has made a confident diagnosis, they’ll create a personalised treatment plan because when it comes to skin, there’s no such thing as one-size-fits-all. Treating a rash isn’t simply a matter of handing over a tube of cream and sending you on your way. A well-designed plan takes into account several important factors, such as your age, medical history, the severity and type of rash, any underlying conditions, and even your skin type or lifestyle.
Here are some of the treatment options your dermatologist may recommend:
- Prescription creams or ointments: These are often the first line of treatment, especially for inflammatory skin conditions like eczema, psoriasis, or allergic dermatitis. Prescription-strength topical corticosteroids, antifungals, or immunomodulators can deliver more targeted and effective results than over-the-counter options. In some cases, dermatologists may also recommend medicated moisturisers to repair the skin barrier and reduce irritation.
- Oral medications: For rashes that are more widespread, severe, or unresponsive to topical treatments, oral medication might be necessary. This could include antihistamines for allergic reactions, antibiotics for bacterial infections, antifungal pills for deep fungal infections, or even immune-suppressing drugs in autoimmune conditions. The goal is to treat the cause internally when topical products alone aren’t enough.
- Lifestyle and environmental changes: Your dermatologist may also suggest adjustments to your daily routine to prevent future flare-ups. For instance:
- Switching to fragrance-free or hypoallergenic skincare products
- Avoiding known allergens like certain metals, fabrics, or foods
- Changing your laundry detergent or shampoo
- Installing a humidifier during dry seasons
- Reducing stress, which is a common trigger for many skin conditions
- Ongoing follow-up: If your rash is chronic, recurs frequently, or is part of a more complex condition, follow-up appointments will be important. Dermatologists monitor how your skin responds to treatment and may adjust the plan over time. They’ll also help you learn how to manage your condition long-term to minimise flare-ups and prevent complications like scarring or secondary infections.
Ultimately, the goal is not just to clear up the rash, but to prevent it from coming back and to keep your skin as healthy and resilient as possible.
When to See a Dermatologist
Not all rashes need an emergency visit but knowing when to seek professional help can make a huge difference. While many rashes improve on their own or respond to basic care, some can linger, worsen, or signal an underlying condition that needs medical attention. A dermatologist’s expertise ensures you get the right diagnosis and the right treatment, sooner rather than later.
You should consider booking an appointment with a dermatologist if:
- The rash has lasted longer than two weeks: Most mild skin irritations clear up in a week or so with over-the-counter creams and home care. If yours hasn’t improved or has actually gotten worse it’s time to get it checked.
- The rash is spreading, changing, or behaving unpredictably: A rash that rapidly expands, changes colour or texture, or starts forming blisters or open sores should not be ignored. This can indicate anything from an allergic reaction to an infection, or even a systemic condition that needs further testing.
- You have a fever, pain, or other symptoms along with the rash: Rashes that come with additional symptoms such as fever, joint pain, swollen lymph nodes, or fatigue can be signs of a serious illness. These could range from viral or bacterial infections to autoimmune disorders.
- Over-the-counter treatments aren’t working: If you’ve tried creams, antihistamines, or moisturisers and nothing seems to be helping or if your symptoms keep coming back it’s time for a deeper investigation. You might need prescription treatments or further testing to uncover the root cause.
- The rash is affecting your quality of life: Constant itching, discomfort, or concern about appearance can have a real impact on your mental health and daily functioning. A dermatologist can help ease your symptoms, restore your confidence, and prevent long-term skin damage.
- You’re unsure about the cause and want clarity: Sometimes peace of mind is reason enough. Skin conditions often look similar, and misdiagnosis through online searches or trial-and-error treatments can waste time and worsen the situation. Getting expert advice early means fewer complications, faster healing, and better long-term skin health.
Bottom line: If something feels off, don’t wait it out or self-diagnose especially if your rash is persistent, painful, or confusing. Seeing a dermatologist early can lead to more effective treatment, prevent infections or scarring, and catch any serious conditions while they’re still manageable.
Final Thoughts: Don’t Leave Rashes to Guesswork
Rashes may be common, but they shouldn’t be ignored. A qualified dermatologist doesn’t just treat the skin they investigate what your skin might be trying to tell you about your health.
If you’re uncertain about a rash or simply want expert reassurance, don’t hesitate to book a consultation with one of our experienced dermatologists.
References:
- Mockenhaupt, M., Viboud, C., Dunant, A., et al. (2008). Stevens–Johnson syndrome and toxic epidermal necrolysis: assessment of medication risks with emphasis on recently marketed drugs. Journal of Investigative Dermatology, 128(1), 35–44. DOI: 10.1038/sj.jid.5701033. Available at PubMed: https://pubmed.ncbi.nlm.nih.gov/17805350/
- Johansen, J.D., Aalto‑Korte, K., Agner, T., et al. (2015). European Society of Contact Dermatitis guideline for diagnostic patch testing – recommendations on best practice. Contact Dermatitis, 73(4), 195–221. DOI: 10.1111/cod.12432. Accessible via ResearchGate: https://www.researchgate.net/publication/280114601_European_Society_of_Contact_Dermatitis_guideline_for_diagnostic_patch_testing_-_Recommendations_on_best_practice
- Simonsen, A.B., Andersen, K.E., Veien, N.K., et al. (2018). Contact dermatitis and patch testing for the allergist. Annals of Allergy, Asthma & Immunology, 120(6), 592–598. Available via journal: https://www.annallergy.org/article/S1081-1206(18)30163-7/fulltext
- Schwartz, R.A., McDonough, P.H., Lee, B.W. (2013). Toxic epidermal necrolysis: Part II. Prognosis, sequelae, diagnosis, differential diagnosis, prevention, and treatment. Journal of the American Academy of Dermatology, 69(2), e103–e118. Accessible through Wikipedia reference: https://en.wikipedia.org/wiki/Toxic_epidermal_necrolysis
- Roujeau, J.-C., Kelly, J.P., Naldi, L., et al. (1995). Medication use and the risk of Stevens–Johnson syndrome or toxic epidermal necrolysis. The New England Journal of Medicine, 333(24), 1600–1607. DOI: 10.1056/NEJM199512143332404. PubMed Abstract: https://pubmed.ncbi.nlm.nih.gov/7477195/
