If you’ve noticed thickened skin, swelling, or an enlarged shape developing around your nose, your first thought might be rosacea or rhinophyma. After all, rhinophyma is widely known as the severe, nose-altering form of rosacea. But what many people don’t realise is this: not every swollen or bulbous nose is actually rhinophyma.
Your symptoms might look like rhinophyma, but several other skin and connective tissue disorders can mimic it closely. That’s where misdiagnosis happens and that’s also where the real problems begin. When you’re treated for the wrong condition, your symptoms may worsen, your self-confidence may take a hit, and the true underlying issue continues untreated.
So in this article, I’ll walk you through why rhinophyma is sometimes misdiagnosed, which other conditions resemble it, how dermatologists tell the difference, and what steps help you move towards the right diagnosis. You’ll also learn why imaging, biopsy, and specialist assessment are so important especially if you’re considering help from a trusted rhinophyma clinic in London.
Let’s start by understanding what rhinophyma actually is and why it gets confused with other conditions so often.
What Rhinophyma Really Is
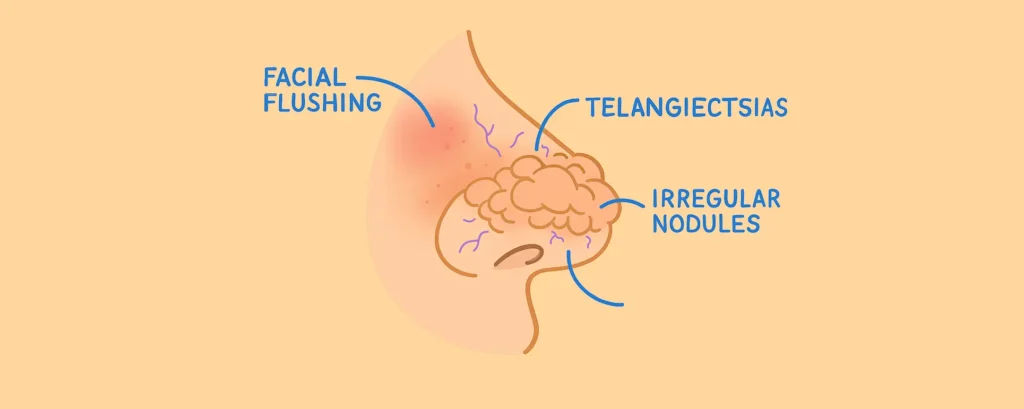
Rhinophyma develops when the skin on your nose becomes thick, swollen, bumpy, and enlarged. You can think of it as the extreme end of rosacea, although newer research shows that not everyone with rhinophyma has active rosacea symptoms.
The key features include:
- A bulbous or rounded nose shape
- Thickened, uneven, nodular skin
- Large or visible pores
- Redness due to increased blood vessels
- Excess growth of sebaceous (oil) glands
Because rhinophyma changes the structure of your skin itself, it can be distressing. You may feel self-conscious in photos, during conversations, or even when looking in the mirror. But the frustration only grows when you don’t know if the diagnosis is accurate.
That’s why it’s so important to understand that other conditions can mimic these exact symptoms.
Why Rhinophyma Is Often Misdiagnosed
Rhinophyma sits at an intersection of several medical fields dermatology, autoimmune medicine, and plastic surgery. It involves redness, swelling, tissue growth, and vascular changes that overlap with many disorders.
You may be misdiagnosed because:
- Your symptoms look visually similar to unrelated conditions.
- Early rhinophyma can be subtle and vague.
- Not all doctors specialise in complex facial skin disorders.
- Some conditions require deeper testing beyond visual inspection.
- Many people seek help late, when symptoms have advanced.
A misdiagnosis might mean you’re prescribed rosacea creams, antibiotics, or laser sessions that won’t help if your condition isn’t actually rosacea-related. The wrong treatment doesn’t just waste time it may also cause worsening of symptoms or irreversible changes.
That’s why dermatologists rely on differential diagnosis, which means ruling out other diseases with similar appearances before confirming rhinophyma.
Let’s explore the conditions that most often get confused with it.
Conditions That Mimic Rhinophyma
Below are the main disorders that resemble rhinophyma some visually, some through similar tissue growth, and some through overlapping inflammation patterns.
1. Lupus (Especially Lupus Pernio)
You may know lupus as an autoimmune disease that affects multiple organs, but the skin can also be heavily involved.
Lupus pernio, a chronic skin form of lupus, can cause:
- Purple or red swelling around the nose
- Thickened skin
- Persistent facial lesions
- Changes that slowly enlarge over time
These symptoms can look almost identical to rhinophyma from a distance.
Key differences dermatologists watch for:
- Lupus swelling is often firmer than rosacea-related thickening.
- The colour has a bluish-purple tone rather than pink or red.
- Lupus pernio often affects the cheeks and ears as well.
- Blood tests may show autoimmune markers like ANA or ACE levels.
This type of condition requires specialist autoimmune treatment, not traditional rhinophyma procedures.
2. Sebaceous Hyperplasia
Sebaceous hyperplasia involves overgrowth of oil glands on the skin. You may notice:
- Yellowish, soft bumps
- Enlarged pores
- Greasy texture
- Symmetrical clusters of small nodules
When this happens in large numbers around the nose, it can mimic early rhinophyma. But the growth pattern is different.
How dermatologists differentiate it:
- Sebaceous hyperplasia causes smaller bumps, not large deformities.
- Pressing lightly can show a central depression in each lesion.
- Dermatoscopy (skin microscope) helps identify the uniform oil-gland pattern.
Unlike rhinophyma, it rarely reshapes the entire nose.
3. Granulomatous Disorders
Conditions such as sarcoidosis, granulomatosis with polyangiitis, or granulomatous rosacea can cause swelling that resembles rhinophyma.
What granulomatous disorders look like:
- Firm nodules under the skin
- Reddish-brown swelling
- Patchy, irregular thickening
- Pain or tenderness in some cases
The major difference:
Granulomas affect deeper layers of the skin and often appear in multiple facial areas not only the nose.
A biopsy usually reveals the granulomas responsible for the swelling.
4. Basal Cell Carcinoma (Skin Cancer)
This one surprises many people. Certain slow-growing skin cancers can mimic rhinophyma’s bumpy texture.
Skin-cancer-like signs include:
- A pearly or shiny bump
- Slow expansion of a nodule
- Tiny blood vessels on the surface
- A sore that doesn’t fully heal
In later stages, it can create distortions that resemble rhinophyma’s thickened shape.
Why this misdiagnosis is dangerous:
Delaying cancer treatment gives it time to grow deeper or spread locally, increasing the complexity of future surgery.
5. Chronic Infections
Long-standing local infections, especially fungal or bacterial ones, can cause persistent inflammation and swelling around the nose.
Common infection-based symptoms:
- Redness
- Heat
- Tenderness
- Thickened texture in recurrent cases
Because the changes develop slowly, they may resemble early rhinophyma but require a completely different treatment approach.
6. Rosacea Without Rhinophyma
Some patients have redness and swelling that look worse than typical rosacea but haven’t progressed into true rhinophyma.
This situation can create confusion for both patients and general practitioners.
What dermatologists check for:
- Whether there is tissue overgrowth
- Whether pores have enlarged
- Whether skin texture has changed permanently
Without structural thickening, the condition isn’t rhinophyma even if it feels severe.
How Dermatologists Tell the Difference

If your nose swelling isn’t clearly explained by visual signs alone, a dermatologist may use several tools to make an accurate diagnosis. That’s because guessing isn’t good enough the right diagnosis changes everything about your treatment plan.
Here’s how specialists differentiate between rhinophyma and its look-alikes.
1. Advanced Clinical Examination
A detailed exam helps your dermatologist understand:
- Whether swelling is soft or firm
- Whether skin texture has changed
- Whether pores are enlarged
- What type of blood vessels are visible
- Whether the condition is symmetrical or uneven
The shape and surface of the nose give important diagnostic clues.
2. Dermatoscopy
A dermatoscope lets the dermatologist see the surface of the skin in high detail.
It helps identify:
- Sebaceous hyperplasia patterns
- Cancer-related blood vessels
- Rosacea-specific vascular changes
- Follicle plugging
- Nodular formations
This tool alone can prevent many misdiagnoses.
3. Imaging (CT or MRI)
Not everyone needs imaging, but it’s used when deeper conditions are suspected.
Imaging helps:
- Detect granulomas
- Map the thickness of tissues
- Rule out tumour growth
- Evaluate deformity patterns
- Guide surgical planning
If your swelling is unusual or progressing fast, imaging becomes even more important.
4. Biopsy
A biopsy is the gold-standard tool when diagnosis is uncertain.
It allows dermatologists to:
- Identify granulomas
- Detect cancer cells
- Confirm sebaceous gland overgrowth
- Identify autoimmune involvement
Biopsy results can completely change the direction of your treatment.
5. Blood Tests
Blood tests help rule out autoimmune conditions or chronic inflammation.
Examples include:
- ANA levels (lupus indicator)
- ACE levels (sarcoidosis indicator)
- Inflammatory markers
These tests aren’t for everyone, but they’re used when swelling behaves in a way that doesn’t match classic rhinophyma.
Why Misdiagnosis Matters So Much
Rhinophyma is a structural condition. Other look-alike disorders may be inflammatory, autoimmune, cancerous, or infectious.
When you’re misdiagnosed:
- The wrong treatments are applied.
- The real condition progresses.
- You may develop permanent skin changes.
- Your nose shape may become harder to treat.
- Emotional and social confidence may decline.
The earlier you get the correct diagnosis, the better your options become especially when it comes to treatment planning or cosmetic correction.
Treatment Depends Entirely on the Correct Diagnosis
Here’s how different conditions require completely different treatments.
If it’s true rhinophyma:
You may need:
- CO₂ laser reshaping
- Radiofrequency contouring
- Surgical sculpting
- Electrosurgery
- Medication if rosacea is also present
These procedures remove excess tissue and restore a more natural shape.
If it’s lupus pernio:
You’ll likely need:
- Steroids
- Immunosuppressants
- Autoimmune-focused treatment
Cosmetic reshaping comes later, not first.
If it’s granulomatous disease:
Treatment may include:
- Anti-inflammatory medication
- Autoimmune therapy
- Antibiotics or antifungals
Surgery won’t help unless the underlying disorder is treated.
If it’s sebaceous hyperplasia:
Options include:
- Laser
- Electrocautery
- Topical treatments
This condition rarely requires rhinophyma-style sculpting.
If it’s skin cancer:
You need:
- Mohs surgery
- Cancer-focused excision
- Follow-up dermatology care
Delaying cancer treatment is never safe.
If it’s chronic infection:
You may need:
- Antibiotics
- Antifungals
- Anti-inflammatory care
Again rhinophyma treatments won’t help infection-based swelling.
Why You Should See a Specialist Early
If you’re unsure whether your condition is rhinophyma or something else, you deserve clarity. The longer you wait, the harder it becomes to get the result you want.
A specialist can help you:
- Avoid unnecessary treatments
- Receive an accurate diagnosis
- Understand all your options
- Build a personalised plan
- Reduce long-term deformity
If you’re in the UK and want expert evaluation, it’s worth considering a trusted rhinophyma clinic in London with experience in complex differential diagnosis.
FAQs:
1. Can rhinophyma really be misdiagnosed as other conditions?
Yes, it can. Rhinophyma shares several visual features with autoimmune, infectious, and granulomatous conditions, which is why misdiagnosis happens more often than people realise. When a doctor relies purely on appearance without deeper investigation, the thickened skin, redness, and swelling can easily be mistaken for lupus pernio, sarcoidosis, granulomatous rosacea or even chronic infections. This is why dermatologists often combine visual examination with imaging, dermatoscopy and sometimes biopsy to confirm the true cause before starting treatment.
2. How do dermatologists actually confirm that it’s rhinophyma and not something else?
Dermatologists begin with a close clinical examination to understand the nature of the swelling and the texture of the skin. They look for tell-tale signs such as enlarged pores, skin thickening and excess sebaceous tissue. If the symptoms seem unusual or resemble other disorders, they may then use dermatoscopy to view the skin more clearly. In cases where uncertainty remains, they might order imaging to examine deeper structures or perform a biopsy to study tissue under a microscope. This step-by-step approach helps avoid unnecessary treatments and ensures the diagnosis is correct.
3. Why is it dangerous to assume nose swelling is always caused by rosacea or rhinophyma?
Assuming that swelling is rhinophyma can lead to the wrong treatment, which often allows the real condition to worsen. For example, lupus pernio requires immunosuppressive medication, not rosacea creams. Granulomatous diseases may need antibiotics or autoimmune therapy, and skin cancers demand urgent surgical intervention. If you receive the wrong treatment, the underlying condition continues to progress silently, and some of these illnesses can cause permanent changes to the nose if left untreated.
4. What symptoms make dermatologists suspect a condition other than rhinophyma?
Dermatologists pay attention to how the swelling feels, how it behaves and how quickly it develops. If the nose has a bluish-purple colour, they may suspect lupus. If there are firm nodules beneath the surface, a granulomatous disease becomes more likely. If a pearly bump or non-healing sore is present, skin cancer moves to the top of the list. And if the swelling appears alongside symptoms in other parts of the face or body, they begin to investigate autoimmune or infectious causes. Every detail helps refine the diagnosis.
5. Can lupus pernio really look the same as rhinophyma?
It can look remarkably similar at first glance. Both conditions cause swelling and thickening of the nose, which is why many patients assume it’s rosacea-related. However, lupus pernio tends to cause firmer swelling with a cooler, violet-toned colour rather than the warm pink or red of rosacea. It may also extend to the cheeks and ears. Blood tests can reveal autoimmune markers, and biopsy results often show granulomas, which confirm that the cause is lupus rather than rosacea.
6. What happens if granulomatous disorders are mistaken for rhinophyma?
If a granulomatous disorder such as sarcoidosis or granulomatosis with polyangiitis is treated as rhinophyma, the swelling may continue to grow and spread. These conditions involve deep inflammatory nodules that don’t respond to rosacea-focused treatments or laser sculpting. Without the correct therapy, granulomas persist and the tissue becomes more distorted over time. Proper treatment usually requires medication to calm the immune system or treat infection, and this can only be started once the correct diagnosis is made.
7. Is it possible for skin cancer to resemble rhinophyma?
Yes, particularly in its slower, nodular forms. A basal cell carcinoma can create bumps, bleeding spots or thickened patches that resemble rhinophyma. Over time, the nodule may enlarge and change the shape of the nose. This similarity is risky because delaying cancer treatment gives it a chance to invade deeper tissue. A dermatologist can usually spot suspicious patterns using dermatoscopy and confirm the diagnosis with a biopsy, ensuring that cancer is detected early.
8. Can chronic infections cause nose swelling that looks like rhinophyma?
Chronic infections can create long-standing inflammation, redness and thickened skin that closely resemble early rhinophyma. These infections may be bacterial or fungal and often develop slowly, which makes them difficult to distinguish without proper testing. If swelling improves with antibiotics or antifungals, that is often the biggest clue that an infection, not rosacea, was responsible.
9. What should someone do if they’re unsure whether their diagnosis is correct?
If you’re uncertain about your diagnosis or your symptoms don’t match the treatment you’ve been given, it’s always worth seeking a second opinion from a specialist. Dermatologists who deal with complex facial conditions can evaluate the swelling more thoroughly. They may perform a dermatoscopic exam, recommend imaging or order a biopsy to confirm what is truly happening beneath the skin. Getting clarity early helps prevent unnecessary progression and ensures that the right treatment is given from the start.
10. Why does the treatment plan change completely depending on the exact diagnosis?
Each condition that resembles rhinophyma has a different underlying cause. True rhinophyma involves structural changes in the skin and often requires laser surgery or tissue sculpting. Lupus pernio requires targeted immune therapy. Granulomatous diseases often need anti-inflammatory or antimicrobial treatment. Skin cancer requires surgical removal. Infections need antibiotics or antifungals. Because the root cause varies so widely, the right diagnosis determines everything from medical therapy to surgical planning and long-term management. That’s why identifying the correct condition from the start is so important.
Final Thoughts: Why Getting the Right Diagnosis Matters
When nose swelling or thickening starts to worry you, it’s natural to jump straight to rhinophyma as the explanation. But as you’ve seen throughout this guide, several conditions from lupus pernio to granulomatous disorders and even skin cancer can look almost identical on the surface. That’s why the most important step you can take is getting an accurate diagnosis before starting any treatment.
The right diagnosis protects you from wasted time, unnecessary procedures and worsening symptoms. It also opens the door to a treatment plan that’s actually designed for your condition, not just what it resembles on the outside. So if you’re feeling unsure, or if you want a clearer understanding of what’s really causing the changes in your nose, seeing a specialist early makes a world of difference.
If you’re considering Rhinophyma clinic in London, you can contact us at London Dermatology Centre to book a consultation with one of our specialists. You’ll receive a thorough evaluation, clarity about your condition and guidance on the safest, most effective next steps.
References:
1. Dick, M.K. & Patel, B.C. (2023) ‘Rhinophyma’, StatPearls [Internet], Treasure Island (FL): StatPearls Publishing. Available at: https://www.ncbi.nlm.nih.gov/books/NBK544373/
2. Trokhan, E.Q. (2004) ‘Destructive lupus pernio masquerading as rhinophyma in a patient with sarcoidosis’, Journal of the American Academy of Dermatology, 50(4), pp. 643-646. Available at: https://www.jaad.org/article/S0190-9622(03)03494-7/fulltext
3. Koneti, J. et al. (2022) ‘Sarcoidosis and its dermatological manifestations: a narrative review’, International Journal of Dermatology, 61(2), pp. 130-142. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9481194/
4. Saleem, M.D., Oussedik, E. & Jorizzo, J.L. (2013) ‘Medical Treatment of Rosacea’, Dermatology Research and Practice, 2013, pp. 1–7. MDPI. Available at: https://www.mdpi.com/1422-0067/21/22/8631
5. Lallas, A., Kyrgidis, A. & Tzellos, T. (2020) ‘Clinical Diagnosis and Management of Rosacea: A Review’, Journal of Clinical Medicine, 9(6), p.1858. MDPI. Available at: https://www.mdpi.com/2077-0383/9/6/1858
