Introduction: Flakes, Itch, and Confusion
It’s easy to mistake scalp psoriasis for dandruff. Both can cause itching, flaking, and discomfort—but the underlying causes and treatments differ significantly. Dandruff is often a mild, manageable condition, while scalp psoriasis is a chronic autoimmune disorder that can be more severe and persistent. Misdiagnosing one for the other can lead to ineffective treatment and prolonged discomfort. In this article, we’ll break down the differences between the two, explore their causes, symptoms, and triggers, and explain how dermatologists diagnose and manage scalp psoriasis. Whether you’re dealing with stubborn flakes or irritated skin, understanding what you’re up against is the first step to finding relief.
What Is Dandruff?
Dandruff, also known as seborrhoeic dermatitis in more severe cases, is a common scalp condition that leads to white or yellow flakes of dead skin. It can cause mild itchiness and redness, but it’s generally harmless and not contagious. The exact cause of dandruff isn’t fully understood, but it’s often linked to an overgrowth of Malassezia, a yeast-like fungus that lives on the scalp. Other contributing factors include oily skin, stress, hormonal changes, and even cold weather. Most people experience dandruff at some point in their lives, and it can usually be managed with over-the-counter shampoos containing ingredients like zinc pyrithione, ketoconazole, or salicylic acid.

What Is Scalp Psoriasis?
Scalp psoriasis is an autoimmune condition in which skin cells multiply too quickly, leading to thick, scaly patches that can appear anywhere on the scalp—and sometimes beyond the hairline. Unlike dandruff, scalp psoriasis causes silvery-white scales, reddish plaques, and sometimes painful itching or burning. It’s part of a larger group of conditions under the umbrella of psoriasis and may also appear on elbows, knees, or other areas of the body. The condition isn’t caused by poor hygiene or fungal overgrowth, but by an overactive immune response. It can be mild or severe and often runs in families. Treatment typically requires prescription-strength shampoos, topical steroids, or even systemic medication.
Key Differences in Appearance
One of the clearest ways to tell dandruff and scalp psoriasis apart is by looking closely at the scalp. Dandruff usually results in fine, oily white or yellow flakes that come off easily. The skin underneath may be slightly red but not thickened. In contrast, scalp psoriasis produces thicker, dry scales that may be silvery in colour and are often tightly packed or stuck to the skin. The underlying patches of skin can be red and inflamed, and in some cases, the plaques extend beyond the scalp, especially around the neck or ears. If your flakes are persistent, painful, or accompanied by inflamed skin, it may be time to see a dermatologist.
Itch and Discomfort: Similar but Not the Same
Itching is common in both dandruff and scalp psoriasis, but the intensity and accompanying sensations may differ. Dandruff-related itch is typically mild and comes and goes. In contrast, scalp psoriasis can cause intense itching that interferes with sleep or daily activities. Some people describe a burning or stinging sensation in addition to the itch. Excessive scratching can lead to bleeding or even infection in both conditions, but this risk is particularly high in untreated scalp psoriasis. If your itching feels more like a deep discomfort or is accompanied by soreness or tightness in the skin, it may signal something more serious than simple dandruff.
Triggers and Risk Factors
Dandruff is often triggered by external factors like stress, cold weather, dry air, or infrequent shampooing. Oily skin can also contribute to the condition, creating an environment where Malassezia thrives. Scalp psoriasis, on the other hand, is linked to internal immune system dysfunction. Common triggers include stress, infections, certain medications, and injury to the skin (known as the Koebner phenomenon). Genetics play a strong role—if you have a family member with psoriasis, your chances of developing it increase. Understanding your personal triggers is crucial for both conditions, as it helps manage flare-ups and supports a longer-term treatment strategy.
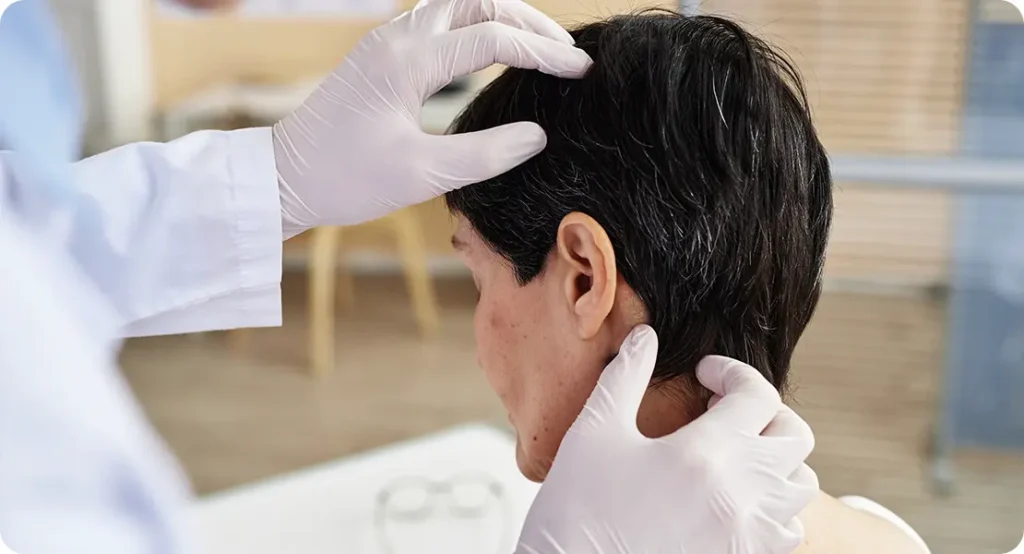
How a Dermatologist Diagnoses the Condition
Diagnosis starts with a thorough examination of the scalp. A dermatologist may look at the size, shape, colour, and distribution of the flakes and patches. In some cases, they might gently scrape the scales to observe the underlying skin. If the diagnosis is unclear, a skin biopsy may be taken for lab analysis. For dandruff, a diagnosis is usually straightforward and based on clinical signs. Psoriasis may require further investigation, especially if other parts of the body are affected. It’s important to avoid self-diagnosing—what looks like dandruff might be something more serious requiring medical intervention.
Treatment for Dandruff
Dandruff can often be managed effectively with the right shampoo. Active ingredients to look for include zinc pyrithione (antifungal), ketoconazole (antimicrobial), selenium sulphide (slows cell turnover), salicylic acid (helps remove flakes), and coal tar (reduces inflammation). Regular washing is key, and some people may need to rotate between different products to maintain results. Lifestyle changes, such as reducing stress, improving diet, and keeping the scalp clean, can also help. In rare cases, more persistent dandruff may require prescription shampoos or creams, but for most, a few weeks of targeted care leads to noticeable improvement.
Treatment for Scalp Psoriasis
Managing scalp psoriasis usually requires a more intensive and long-term approach. Topical corticosteroids are often prescribed to reduce inflammation and slow cell turnover. These may come as lotions, foams, or medicated shampoos. Vitamin D analogues like calcipotriol are also used to regulate skin cell production. For more severe cases, systemic medications—such as methotrexate or biologics—may be needed. Phototherapy (light treatment) can also help some patients. Unlike dandruff, scalp psoriasis tends to return, so ongoing management is essential. A dermatologist will tailor treatment based on the severity of symptoms, patient preference, and response to previous therapies.
Can You Have Both?
Yes—it’s entirely possible to have both dandruff and scalp psoriasis. In fact, some patients initially present with symptoms of one, only to later develop the other. This overlap can make diagnosis and treatment trickier, which is why seeing a dermatologist is so important. A tailored treatment plan may include antifungal shampoos for dandruff and corticosteroid solutions for psoriasis. Managing both conditions at once often involves alternating therapies and paying close attention to which symptoms flare up when. If you’re using one treatment and not seeing results, it may be because there’s an underlying condition that hasn’t been fully addressed.
Lifestyle Tips for Scalp Health
Regardless of which condition you have, there are steps you can take to improve your scalp health. Avoid scratching—even when itching is intense—as it can worsen inflammation and lead to infection. Choose gentle, fragrance-free hair products and avoid harsh styling practices. Manage stress levels, as both dandruff and psoriasis are known to flare during emotional upheaval. A balanced diet rich in anti-inflammatory foods—like omega-3 fatty acids, green leafy vegetables, and berries—may also support skin health. Finally, keep your scalp clean, but don’t over-wash, as that can strip natural oils and trigger irritation.
When to See a Dermatologist
If you’ve tried over-the-counter shampoos for weeks with little improvement, or if your symptoms are worsening, it’s time to consult a dermatologist. Redness that spreads beyond the scalp, painful plaques, bleeding, or intense itch are warning signs that you’re dealing with more than dandruff. A dermatologist can offer a firm diagnosis, prescribe targeted treatments, and help you avoid complications. They’ll also rule out other scalp conditions like eczema, fungal infections, or even lichen planopilaris, which can mimic symptoms of dandruff or psoriasis. Early treatment leads to better outcomes, so don’t wait too long to seek professional help.

Impact on Hair and Scalp Condition
Scalp psoriasis and dandruff don’t just affect the skin—they can impact the condition of your hair, too. With dandruff, hair quality is usually unaffected, though excessive scratching or product buildup may cause temporary dullness. Scalp psoriasis, however, can lead to noticeable hair thinning. This isn’t due to direct follicle damage, but rather inflammation and repeated trauma from scratching or harsh treatments weakening the roots. In some cases, plaques make grooming difficult, leading to tangling or breakage. Fortunately, this hair loss is often temporary and reversible once the inflammation subsides. Gentle care, avoiding heat tools, and using dermatologist-recommended treatments can help preserve hair health while managing symptoms. If you notice excessive shedding, mention it during your dermatology consultation—especially if redness, flaking, or discomfort are also present. Catching the issue early allows for quicker intervention and less disruption to your hair’s natural growth cycle.
Emotional and Psychological Effects
Living with a visible scalp condition can take a toll on your mental health. Dandruff, while mild, can cause embarrassment, particularly when flakes appear on dark clothing or during close social interactions. Scalp psoriasis, being more severe and persistent, often carries a heavier emotional burden. Many sufferers report feelings of self-consciousness, anxiety, or depression—especially if symptoms are difficult to hide. Unlike conditions that can be covered with clothing, the scalp is often exposed during everyday activities like haircuts or swimming. The discomfort from itching, along with the constant need to manage flare-ups, can also lead to sleep disturbances and fatigue. If you’re feeling overwhelmed or socially withdrawn, you’re not alone. It’s important to address the emotional aspects of scalp conditions alongside the physical ones. Talking to a healthcare provider, joining support groups, or speaking with a mental health professional can offer valuable support and coping strategies as part of a holistic approach to care.

Children and Scalp Conditions
Scalp issues aren’t limited to adults—both dandruff and scalp psoriasis can appear in children. Dandruff in children may be linked to hormonal changes during puberty, but can also occur earlier due to dry skin or sensitivity to shampoo. In younger patients, it’s often mistaken for cradle cap, a form of seborrhoeic dermatitis seen in babies. Scalp psoriasis in children tends to present similarly to adults, though it may be misdiagnosed as eczema or a fungal infection. Diagnosis can be more difficult in children, especially if they can’t describe symptoms like burning or itching clearly. If you notice persistent flaking, redness, or scaling on your child’s scalp—especially if it resists treatment—it’s worth seeking specialist advice. Early intervention can prevent discomfort, minimise emotional distress, and avoid long-term scalp damage. Treatments for children are usually gentler, with options like tar-based shampoos, low-strength corticosteroids, and non-medicated emollients forming the first line of care.
Misconceptions and Myths
There are plenty of myths surrounding both dandruff and scalp psoriasis, often leading to confusion or inappropriate treatment. One common misconception is that poor hygiene causes dandruff—this simply isn’t true. Dandruff is more about scalp biology and yeast overgrowth than how often you wash your hair. Another myth is that scalp psoriasis is contagious, which it absolutely is not. People sometimes worry that flakes or plaques can spread through contact, but this fear is unfounded. Some also wrongly believe you should avoid washing your hair during a flare-up. In fact, regular, gentle cleansing is important for both conditions, provided the products used are suitable. Others think natural oils or herbal remedies alone can cure scalp psoriasis, but while they may soothe symptoms, they can’t replace medically proven treatments. Clearing up these myths is essential—not just for those suffering, but for reducing stigma and encouraging more people to seek proper care.
Long-Term Management and Monitoring
Both dandruff and scalp psoriasis benefit from long-term management rather than one-off treatments. While dandruff may come and go, especially with seasonal changes, regular use of medicated shampoos and scalp-friendly hair care can keep it under control. For scalp psoriasis, long-term care often involves maintenance treatments to prevent relapses. This could include rotating topical treatments, ongoing use of tar or salicylic acid shampoos, or even low-dose biologics in more stubborn cases. Regular dermatology check-ups help monitor flare-ups and adjust treatment plans as needed. Keeping a symptom diary can also help track what triggers flare-ups—be it stress, new hair products, or changes in weather. It’s also important to reassess your treatment every few months, as your scalp’s needs may change over time. With professional guidance, consistency, and a bit of patience, both conditions can be well-managed, allowing you to get on with life without constantly worrying about flakes or inflammation.
When Over-the-Counter Remedies Aren’t Enough
Many people start with over-the-counter (OTC) shampoos and treatments at the first sign of flaking, but these aren’t always effective—especially if scalp psoriasis is the cause. OTC products can help mild dandruff, but they usually don’t provide enough relief for moderate to severe psoriasis. If medicated shampoos haven’t helped or symptoms are worsening, it’s time to see a dermatologist. They can prescribe stronger treatments like topical steroids, immunomodulators, or light therapy. Hoping the problem will resolve on its own often delays proper care and increases discomfort. A timely diagnosis and the right treatment plan can make a big difference in both symptom control and quality of life.
Seasonal Changes and Their Impact
Both dandruff and scalp psoriasis can worsen with changes in the seasons, particularly during the colder months. Winter air tends to be dry, which strips moisture from the scalp and increases flaking, irritation, and itchiness. People often wash their hair less frequently in winter, which can exacerbate oil buildup or plaque formation. Summer, on the other hand, may offer temporary relief for some, especially those with scalp psoriasis, thanks to the anti-inflammatory effects of natural sunlight. However, increased sweating and exposure to harsh hair products or chlorine from pools can also trigger flare-ups. Understanding how your scalp reacts to seasonal shifts helps in adjusting your hair care routine and treatment accordingly—whether that means moisturising more, switching shampoos, or using scalp-friendly sunscreens.
The Role of Diet and Lifestyle
Your lifestyle habits, including diet, can influence scalp health. While diet alone won’t cause or cure dandruff or psoriasis, certain foods may trigger inflammation or yeast overgrowth. High-sugar, high-fat diets, or excessive alcohol intake can make flare-ups worse—especially for those with psoriasis. On the flip side, foods rich in omega-3 fatty acids (like salmon and flaxseed), antioxidants (such as berries and leafy greens), and vitamin D may help reduce inflammation. Staying hydrated, managing stress, and getting regular sleep are equally important, as stress is a major trigger for scalp psoriasis. Lifestyle isn’t a replacement for medical treatment, but it plays a supporting role in managing symptoms and reducing frequency of flare-ups over time. Small changes often lead to noticeable improvements.

Final Thoughts: Know What You’re Dealing With
Understanding the difference between dandruff and scalp psoriasis is crucial for choosing the right treatment and getting relief. While the symptoms may look similar at a glance, the causes, treatments, and long-term outlook are very different. Dandruff is common, easily managed, and rarely a sign of something serious. Scalp psoriasis, however, is a chronic condition that needs medical attention and long-term care. If in doubt, don’t guess—speak to a dermatologist. With the right diagnosis and a tailored treatment plan, you can reduce symptoms and improve your scalp health significantly. After all, clarity is the first step towards effective care.
If you are suffering from scalp issues or psoriasis, you can get in touch with us at The London Dermatology Centre to consult with one of our expert dermatologists.
References:
- Mayo Clinic, 2022. Scalp psoriasis. [online]
- NHS, 2023. Dandruff. [online] Available at: https://www.nhs.uk/conditions/dandruff/ [Accessed 14 May 2025].
- American Academy of Dermatology Association, 2023. Scalp psoriasis: Diagnosis and treatment. [online]
- Borda, L.J. and Wikramanayake, T.C., 2015. Seborrheic dermatitis and dandruff: a comprehensive review. Journal of Clinical and Investigative Dermatology, 3(2), pp.1–10.
- National Psoriasis Foundation, 2023. Managing scalp psoriasis. [online]
