Eczema is often described as a condition of dry, inflamed skin, but this explanation only scratches the surface. Over the past decade, research has increasingly shown that the microorganisms living on the skin play a central role in how eczema behaves, flares, and persists.
Many people with eczema experience repeated cycles of improvement and relapse, even when they follow treatment plans carefully. This pattern has led researchers to explore whether changes in the skin microbiome are simply a consequence of eczema or whether they actively drive the disease.
In this article, we explore what microbiome dysbiosis means in eczema, how barrier disruption and microbial imbalance interact, and whether targeting the microbiome can meaningfully alter the long-term course of eczema.
What the Skin Microbiome Really Is
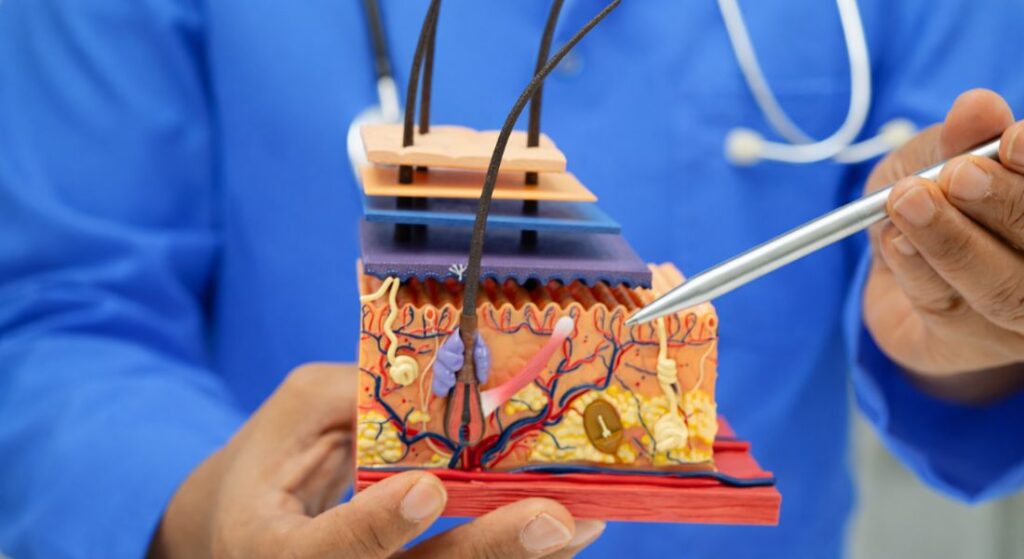
We describe the skin microbiome as the community of bacteria, fungi, and viruses that naturally live on the skin surface. In healthy skin, these microorganisms exist in balance and support normal skin function. They form part of the skin’s first line of defence.
We understand that these microbes interact constantly with the skin barrier and immune system. This interaction helps regulate inflammation and protects against harmful pathogens. The relationship is active and responsive, not passive.
We also recognise that the microbiome is dynamic rather than fixed. It changes in response to environment, skincare, health, and treatment. Maintaining balance is therefore more important than eliminating microbes entirely.
Why the Microbiome Matters in Eczema
We see clear evidence that eczema is associated with disruption of the normal skin microbiome. The balance between protective and harmful organisms becomes altered. This loss of balance plays a direct role in flare development.
We know from research that microbial diversity is reduced in eczema-prone skin. At the same time, certain organisms increase disproportionately. This imbalance is clinically described as dysbiosis.
We now recognise dysbiosis as a defining feature of active eczema rather than a secondary effect. It contributes to inflammation, barrier damage, and symptom persistence. Addressing this imbalance is therefore clinically relevant.
The Central Role of Staphylococcus aureus
In eczema, bacterial balance on the skin plays a critical role in driving inflammation. One organism in particular, Staphylococcus aureus, is closely linked to flare activity and disease severity. Understanding this relationship helps explain why eczema can become persistent and difficult to control.
Staphylococcus aureus is central to eczema because:
- It is commonly present in active eczema – The bacteria is found on the skin of most people during flares, often at much higher levels than on unaffected skin.
- Bacterial load correlates with severity – Higher levels are associated with increased inflammation, itching, and visible skin damage.
- Its role goes beyond colonisation – S. aureus actively disrupts the skin barrier and amplifies immune responses rather than simply living on the surface.
- It drives both flares and persistence – The bacteria contributes to flare initiation and makes it harder for the skin to settle once inflammation has begun.
By recognising the central role of S. aureus, we can take a more targeted approach to managing eczema and supporting long-term skin stability.
Why Staphylococcus aureus Thrives in Eczema Skin
In eczema, we see fundamental disruption of the skin barrier, which changes how the skin interacts with microbes. Cracks in the barrier expose binding sites that bacteria can easily attach to. At the same time, the skin’s natural antimicrobial defences are reduced.
We also recognise that moisture imbalance and chronic inflammation create favourable conditions for bacterial growth. Instead of acting as a protective surface, the skin becomes more biologically permissive. This allows Staphylococcus aureus to establish itself more easily.
We therefore view bacterial overgrowth as a consequence of barrier failure rather than poor hygiene. Addressing the underlying skin environment is essential. Without restoring barrier function, bacterial control remains limited.
How Staphylococcus aureus Worsens Inflammation
Staphylococcus aureus actively contributes to inflammation rather than simply coexisting on the skin. It releases toxins that stimulate immune cells and trigger inflammatory signalling pathways. These responses intensify redness, itching, and tissue damage.
We understand that these toxins also disrupt normal immune regulation. Instead of resolving inflammation, the immune system remains persistently activated. This prolongs flares and increases skin sensitivity.
Over time, this interaction creates a self-perpetuating inflammatory cycle. Bacterial activity fuels inflammation, and inflammation further weakens the skin barrier. Breaking this loop is a key aim of effective eczema management.
Why Scratching Amplifies Microbiome Imbalance
Scratching may feel instinctive, but it has powerful effects on skin health beneath the surface. Understanding this process helps explain why itch control is central to long-term management, not just symptom relief.
Here’s how scratching worsens microbiome imbalance:
1. Scratching Causes Direct Barrier Damage – Persistent itching leads many people to scratch, causing mechanical injury to the skin. Each episode further weakens an already compromised barrier, making it easier for bacteria to penetrate and spread.
2. Barrier Disruption Encourages Bacterial Overgrowth – Once the barrier is broken, microbes can colonise more easily. This shifts the normal skin microbiome towards imbalance, allowing problematic bacteria to dominate.
3. Dysbiosis Intensifies Inflammation and Itch – As microbial imbalance deepens, inflammation increases. This makes itching more severe, reinforcing the itch–scratch cycle and driving further skin damage.
4. Controlling Itch Protects Long-Term Skin Health – We emphasise that itch control is not only about comfort. Reducing scratching helps preserve the skin barrier and stabilise the microbiome, which is essential for recovery and long-term disease control.
By breaking the itch scratch cycle early, we protect both the barrier and the microbiome. This creates the conditions needed for calmer skin, reduced inflammation, and more sustainable healing over time.
Is Microbiome Dysbiosis a Cause or a Consequence?
This question sits at the centre of how we currently understand eczema. We now recognise that microbiome imbalance does not act in isolation. Instead, it develops alongside barrier weakness and ongoing inflammation.
We see strong evidence that dysbiosis is both a result of skin barrier failure and a contributor to disease progression. Each process reinforces the other over time. This makes eczema a self-sustaining biological cycle rather than a single-trigger condition.
We therefore approach eczema as a combined barrier and microbiome disorder. Separating these elements oversimplifies the condition. Meaningful improvement requires addressing both together rather than treating them independently.
Barrier Dysfunction as the Starting Point
In many patients, eczema begins with an inherent weakness in the skin barrier. Genetic factors, such as reduced filaggrin function, play a significant role. Lipid deficiency and impaired tight junctions further weaken the skin’s protective structure.
We understand that this compromised barrier allows abnormal interaction between microbes and immune cells. Substances that should remain outside the skin gain easier access. This shifts immune responses towards chronic inflammation.
In clinical practice, we often see barrier dysfunction precede visible microbiome imbalance. Once the barrier is weakened, microbial changes follow more easily. This is why early barrier support is so important in long-term control.
How Dysbiosis Prevents Barrier Repair
When the skin’s microbial balance is disrupted, healing becomes much harder to achieve. Dysbiosis does not simply coexist with barrier damage, it actively interferes with recovery. This is why eczema can remain unstable even when moisturisers are used consistently.
Dysbiosis prevents barrier repair because:
- Certain bacteria damage skin cells directly – Toxins released by harmful bacteria can injure keratinocytes and disrupt normal skin renewal.
- Healing becomes slower and less efficient – Repair processes are impaired, not absent, making recovery incomplete or prolonged.
- Lipid production is reduced – Microbial imbalance interferes with the skin’s ability to produce barrier lipids, limiting restoration despite regular moisturiser use.
- Balance is essential for full recovery – Without addressing dysbiosis, barrier repair remains partial and eczema control is harder to achieve.
By restoring microbial balance alongside barrier support, we allow both systems to recover together, which is essential for effective and lasting eczema management.
Why Eczema Flares Are Often Triggered by Infection
We often see eczema flares occur after exposure to bacteria or viruses. Even when there is no clear infection, changes in the skin’s microbial balance can activate the immune system. This makes the skin more reactive and prone to inflammation.
We recognise that, in eczema, the line between simple colonisation and infection is not always clear. Microbes that are usually harmless can provoke a strong immune response. This reaction is driven by barrier weakness rather than infection alone.
We therefore view many flares as immune microbial events rather than straightforward infections. The skin responds to microbial signals more aggressively than it should. This explains why flares can occur without obvious signs of infection.
Why Antibiotics Alone Rarely Solve the Problem
We understand that antibiotics can reduce bacterial load in the short term. They are sometimes necessary when infection is clearly present. However, they do not address the underlying skin barrier dysfunction.
We also know that antibiotics do not restore healthy microbial diversity. In some cases, repeated use can further disrupt the skin microbiome. This may leave the skin more vulnerable once treatment stops.
We often see flares return soon after antibiotic courses end. Without barrier repair and microbiome balance, bacteria can re-establish quickly. This is why antibiotics alone rarely provide lasting control.
The Role of Commensal Bacteria in Healthy Skin
We recognise that healthy skin is supported by beneficial, commensal bacteria. These organisms help regulate inflammation and compete with potentially harmful microbes. They form part of the skin’s natural defence system.
We see that, in eczema, these protective species are often reduced. This loss of diversity allows opportunistic bacteria to dominate more easily. The balance shifts away from protection and towards inflammation.
We therefore place importance on preserving and restoring microbial balance. Supporting commensal bacteria strengthens the skin’s resilience. Healthy skin depends not on sterility, but on a stable and diverse microbiome.
How Microbiome Diversity Protects Against Flares
We understand that greater microbial diversity is linked to milder eczema activity. When many organisms coexist, no single harmful species is able to dominate the skin surface. This balance supports calmer immune signalling.
We see that diverse microbial communities limit overgrowth of organisms such as Staphylococcus aureus. Beneficial microbes compete for space and nutrients while moderating inflammatory responses. This helps reduce flare frequency and intensity.
We therefore view restoration of diversity as an important therapeutic goal. Healthy skin is supported by balance rather than elimination of microbes. Diversity protects against instability and recurrent inflammation.
Do Moisturisers Influence the Microbiome?

Moisturisers play a much bigger role than simple hydration. Their effect on the skin barrier directly influences the balance of microorganisms living on the skin. Understanding this link explains why emollients are central to long-term skin control, not just comfort.
Here’s how moisturisers influence the microbiome:
1. Barrier Repair Shapes the Microbial Environment – We recognise that moisturisers strengthen the skin barrier rather than just adding moisture. A healthier barrier makes it harder for harmful bacteria to penetrate and overgrow.
2. Improved Barrier Function Reduces Inflammation – When moisture loss is controlled, inflammation settles. Lower inflammation creates a more stable environment where microbes are less likely to dominate or trigger flares.
3. Stronger Skin Limits Bacterial Penetration – With intact barrier lipids and structure, microbes remain on the surface where they belong. This helps preserve normal microbial balance rather than allowing deeper colonisation.
4. Moisturisation Acts as a Medical Strategy – We treat regular emollient use as a medical intervention, not a cosmetic step. Supporting the barrier also supports microbiome stability, which is why moisturisation sits at the core of eczema and dermatitis management.
By strengthening the barrier, we indirectly protect the microbiome. This dual effect explains why consistent moisturiser use is essential for calmer skin, fewer flares, and long-term disease control.
Anti-Inflammatory Treatment and Microbial Balance
We know that active inflammation destabilises the skin microbiome. Immune activation alters the surface environment and encourages harmful bacterial behaviour. Reducing inflammation helps restore balance.
We see that topical anti-inflammatory treatments reduce bacterial toxins and immune overreaction. As inflammation settles, microbial diversity can begin to recover naturally. The skin becomes less reactive overall.
We approach inflammation control and microbiome stability as interconnected goals. Treating one supports the other. Long-term control depends on addressing both together.
The Emerging Role of Microbiome-Targeted Therapies
There is growing interest in treatments that work with the skin microbiome rather than against it. These approaches aim to support balance on the skin surface, recognising that healthy skin depends on a stable microbial environment. This marks a shift away from blanket eradication towards more nuanced care.
Microbiome-targeted therapies are gaining attention because:
- They focus on balance rather than elimination – The goal is to support healthy microbial communities instead of removing all bacteria.
- They encourage beneficial organisms – Topical probiotics, bacterial lysates, and microbiome-friendly formulations aim to strengthen protective species on the skin.
- They reflect a shift in treatment philosophy – Supporting the microbiome represents a move towards regenerative and restorative care rather than suppression alone.
- Evidence is promising but still evolving – Research is ongoing, results vary between products, and careful clinical application remains essential.
By using these therapies thoughtfully and alongside established treatments, we can support more resilient skin while the evidence base continues to develop.
Why Probiotics Are Not a Simple Solution
Probiotics are often discussed as a straightforward way to improve skin health, but the reality is more complex. Different products behave very differently on the skin, and results are not always predictable. Understanding these limitations helps set realistic expectations.
Probiotics are not a simple solution because:
- Strains and formulations vary widely – Different organisms, delivery systems, and concentrations lead to inconsistent effects on the skin.
- Many organisms do not persist on the skin – Some strains fail to survive or integrate into existing microbial communities once applied.
- Interaction with the skin is not guaranteed – Certain probiotics do not meaningfully influence the skin barrier or immune response.
- Effectiveness varies across studies – Outcomes differ between products, highlighting the need for careful interpretation of evidence.
For this reason, we approach microbiome-based therapy cautiously. Precision, context, and evidence matter far more than supplementation alone, and effective care relies on targeted, clinically guided strategies rather than simple solutions.
The Risk of Over-Sterilising Eczema Skin

We often see eczema worsen when the skin is over-cleansed or repeatedly exposed to antiseptics. While hygiene matters, excessive sterilisation disrupts the natural skin ecosystem. This imbalance, known as dysbiosis, reduces protective microbial diversity. As a result, the skin becomes more vulnerable rather than more resilient. Clean does not always mean healthy for eczema-prone skin.
When beneficial microbes are stripped away, the skin barrier also suffers. Over-cleansing increases dryness, irritation, and micro-damage to the epidermis. This creates ideal conditions for harmful bacteria to dominate. Instead of preventing infection, aggressive cleansing can intensify inflammation and flare frequency. The barrier and microbiome are closely linked and easily destabilised.
We focus on balance rather than sterility in eczema care. Gentle cleansing supports the microbiome while preserving barrier integrity. Our approach prioritises protection, repair, and controlled hygiene rather than elimination of all microbes. Healthy skin relies on coexistence, not eradication. This balance is central to long-term eczema control.
How Dermatologists Integrate Microbiome Knowledge
We now recognise that eczema management must account for microbiome dynamics. Modern dermatology looks beyond visible symptoms to underlying biological interactions. The skin barrier, immune response, and microbial balance are treated as a single system. Ignoring one element limits treatment success. Integration is key to durable results.
Our treatment plans combine barrier repair, inflammation control, and microbial modulation. Moisturisers, anti-inflammatory therapies, and appropriate hygiene work together. This coordinated approach reduces bacterial overgrowth and stabilises immune activity. Over time, it lowers relapse frequency and flare intensity. Each component supports the others.
This strategy underpins effective eczema treatment in London at specialist clinics. We tailor care based on disease severity, history, and response patterns. By addressing microbiome disruption early, we improve long-term outcomes. Integrated care is no longer optional it is the standard. This reflects the evolving science of eczema management.
Why Eczema Management Must Be Long-Term
We understand that microbiome balance cannot be restored overnight. Eczema is a chronic condition influenced by ongoing environmental and biological factors. Short-term treatment may suppress symptoms but rarely delivers stability. Sustainable control requires continuity rather than reactive care. Long-term planning is essential.
Maintenance therapy protects both the skin barrier and microbial diversity. Regular moisturisation, appropriate anti-inflammatory use, and gentle routines prevent relapse. This ongoing support reduces cumulative skin damage. It also limits opportunities for pathogenic bacteria to dominate. Consistency is more effective than repeated crisis treatment.
We encourage patients to view eczema care as a long-term partnership. Preventive strategies reduce flare severity and frequency over time. With proper maintenance, the skin becomes more resilient. Long-term care supports healthier microbiome patterns. This approach delivers lasting improvement, not temporary relief.
When Microbiome Dysbiosis Signals Severe Disease
We often see persistent dysbiosis in patients with poorly controlled eczema. Low microbial diversity and high bacterial load are warning signs. These patterns are frequently linked to severe or treatment-resistant disease. Symptoms tend to be more widespread and recurrent. This indicates a deeper imbalance.
In such cases, standard treatment may no longer be sufficient. Ongoing inflammation fuels further microbiome disruption, creating a vicious cycle. Secondary infections become more likely. Without intervention, skin integrity continues to decline. Specialist assessment is critical at this stage.
We prioritise early identification of microbiome-related severity. Timely escalation of care improves response and limits long-term damage. Targeted therapies help restore balance and control inflammation. Addressing dysbiosis early prevents disease progression. This proactive approach leads to better outcomes.
The Importance of Personalised Eczema Care
We recognise that microbiome patterns differ between individuals. Genetics, age, climate, lifestyle, and environment all influence skin microbes. No two eczema presentations are identical. Standardised routines often fail to address individual needs. Personalisation improves effectiveness.
Our approach adapts treatment to each patient’s profile. We consider triggers, flare patterns, and response history. Tailored care supports the skin’s unique microbial environment. This reduces unnecessary disruption and improves tolerance. Personalised plans outperform generic regimens.
This philosophy is central to modern dermatology practice. We move away from one-size-fits-all treatment models. Precision care supports long-term stability and better quality of life. Understanding individual microbiome variation enhances results. Personalised management is the future of eczema care.
Why Research Is Changing How We View Eczema
Research has fundamentally reshaped how eczema is understood and managed. Rather than seeing it as a simple skin problem, we now recognise it as a condition involving multiple interconnected biological systems. This shift explains why older, single-focus treatments often fell short.
Here’s how modern research has changed our understanding:
1. Eczema Is a Multifaceted Biological Condition – We no longer view eczema as just dry or sensitive skin. Research shows it involves skin barrier dysfunction, immune dysregulation, and microbiome imbalance, all interacting with one another.
2. Damage in One System Affects the Others – When the skin barrier is weakened, allergens and microbes penetrate more easily. This triggers immune activation and inflammation, which then further damages the barrier and disrupts microbial balance.
3. Microbiome Changes Drive Chronic Flares – As inflammation increases, microbial diversity declines. Pathogenic bacteria become dominant, reinforcing inflammation and making flares more persistent and unpredictable.
4. Treating One Element Alone Is Often Insufficient – Focusing only on dryness, inflammation, or infection rarely leads to lasting control. These overlapping processes must be addressed together to stabilise the condition.
5. Modern Treatment Focuses on Restoring Balance – We now prioritise therapies that support barrier repair, calm immune responses, and stabilise the microbiome. This integrated approach reflects current dermatological practice and leads to more durable outcomes.
This evolving understanding has transformed eczema care. By treating the underlying biology rather than just suppressing symptoms, we aim for longer-term control, fewer flares, and healthier skin over time.
When to Seek Specialist Advice
We advise specialist reassessment when eczema flares repeatedly despite good treatment adherence. Frequent relapses suggest that underlying drivers remain unaddressed. Persistent inflammation is often a sign of deeper barrier or microbiome dysfunction. At this stage, escalation of care becomes important. Early review prevents disease progression.
Ongoing infection, increasing severity, or reduced response to standard therapies are key warning signs. These patterns often reflect microbial imbalance rather than simple irritation. Repeated antibiotic or steroid use without improvement warrants further evaluation. Specialist input helps identify contributing factors. This includes immune activity, barrier integrity, and microbial shifts.
We use specialist assessment to refine long-term management plans. Advanced therapies and tailored strategies improve disease control. Addressing the root causes reduces flare frequency and severity. Expert care supports sustainable outcomes rather than temporary relief. Timely referral plays a critical role in effective eczema management.
FAQs:
1. What does “skin microbiome dysbiosis” mean in eczema?
Skin microbiome dysbiosis refers to an imbalance in the normal community of microorganisms living on the skin. In eczema, this usually means reduced microbial diversity alongside overgrowth of certain bacteria, particularly Staphylococcus aureus. This imbalance alters how the skin barrier and immune system behave, contributing to inflammation, itching, and difficulty maintaining long-term disease control.
2. Is microbiome imbalance the cause of eczema or the result of it?
Current research shows that microbiome dysbiosis is both a cause and a consequence of eczema. Barrier weakness and immune dysfunction allow harmful bacteria to dominate, while bacterial overgrowth further damages the barrier and sustains inflammation. This creates a self-reinforcing cycle, meaning dysbiosis actively contributes to disease persistence rather than being a passive side effect.
3. Why is Staphylococcus aureus so strongly linked to eczema flares?
Staphylococcus aureus plays an active role in eczema by releasing toxins that stimulate immune responses and worsen inflammation. Higher bacterial levels are consistently associated with more severe symptoms, increased itch, and poorer barrier function. Rather than simply living on the skin, this bacterium directly drives flare intensity and prolongs recovery.
4. Does killing bacteria always improve eczema symptoms?
Reducing bacterial load can help in the short term, particularly when infection is present, but killing bacteria alone rarely leads to lasting improvement. Antibiotics do not restore barrier function or microbial diversity, and repeated use may worsen dysbiosis. Sustainable eczema control requires barrier repair, inflammation management, and microbiome stabilisation together.
5. How does scratching affect the skin microbiome in eczema?
Scratching physically damages the skin barrier, creating openings that allow bacteria to spread and dominate. This worsens microbial imbalance and increases inflammation, which in turn intensifies itch. The result is a reinforcing itch–scratch cycle where microbiome dysbiosis and barrier damage continuously fuel each other.
6. Can moisturisers really influence the skin microbiome?
Moisturisers influence the microbiome indirectly by restoring barrier integrity. A stronger barrier reduces inflammation and limits bacterial penetration, creating a more stable environment for healthy microbes. This is why regular emollient use is considered a core medical treatment in eczema rather than a cosmetic measure.
7. Are probiotics effective for treating eczema-related dysbiosis?
Probiotics are not a guaranteed solution for eczema. Many strains do not survive well on the skin or integrate into existing microbial communities, and clinical outcomes vary widely between products. While microbiome-targeted therapies are promising, they require careful selection and should be used alongside established eczema treatments rather than as standalone solutions.
8. Why can eczema flare without obvious infection?
In eczema, even normal skin bacteria can provoke excessive immune responses due to barrier weakness and immune dysregulation. This means flares can occur without signs of overt infection. The skin reacts abnormally to microbial signals, making inflammation possible even when bacteria are merely colonising rather than infecting the skin.
9. Does over-cleansing make eczema and dysbiosis worse?
Excessive cleansing and frequent antiseptic use can worsen eczema by stripping away beneficial microbes and damaging the skin barrier. This loss of microbial diversity leaves the skin more vulnerable to pathogenic overgrowth and inflammation. Gentle cleansing that preserves the microbiome is therefore essential for long-term stability.
10. Can targeting the microbiome change the long-term course of eczema?
Targeting the microbiome can support better long-term control when combined with barrier repair and anti-inflammatory treatment. While microbiome-focused therapies alone are unlikely to cure eczema, stabilising microbial balance reduces flare frequency and supports barrier healing. Long-term improvement depends on addressing all interconnected drivers of the disease rather than focusing on a single factor.
Final Thoughts: Understanding Eczema as a Barrier–Microbiome Condition
Current research makes it clear that eczema is not driven by a single factor. Skin barrier weakness, immune overactivity, and microbiome dysbiosis work together to shape how the condition flares, settles, and persists over time. Reduced microbial diversity and overgrowth of organisms such as Staphylococcus aureus are not just consequences of eczema, but active contributors that interfere with healing and prolong inflammation. Viewing eczema through this combined biological lens helps explain why short-term fixes often fall short and why long-term stability requires a more integrated approach.
If you’re looking for eczema treatment in London, you can reach out to us at London Dermatology Centre to book a consultation with one of our specialists. We focus on personalised care that addresses barrier repair, inflammation control, and microbiome balance together, helping you move towards calmer, more resilient skin with realistic expectations and evidence-based guidance.
References:
1. Wrześniewska, M., Wołoszczak, J., Świrkosz, G., Szyller, H. & Gomułka, K., 2024. The Role of the Microbiota in the Pathogenesis and Treatment of Atopic Dermatitis A Literature Review. International Journal of Molecular Sciences, 25(12), 6539. https://www.mdpi.com/1422-0067/25/12/6539
2. Ahlström, M.G. et al., 2025. Resilience of the Skin Microbiome in Atopic Dermatitis. International Journal of Molecular Sciences, 26(23), 11737. https://www.mdpi.com/1422-0067/26/23/11737
3. Mohammad, S. et al., 2024. Atopic dermatitis: Pathophysiology, microbiota, and metabolome – A comprehensive review. https://www.sciencedirect.com/science/article/pii/S0944501323002987
4. Koh, L.F., 2022. Skin microbiome of atopic dermatitis. This article outlines reduced microbial diversity and overrepresentation of S. aureus in AD skin and discusses implications for immune function and skin health. https://www.sciencedirect.com/science/article/pii/S1323893021001404
5. The role of the skin microbiome in atopic dermatitis: a systematic review (2017) British Journal of Dermatology. https://pubmed.ncbi.nlm.nih.gov/28207943/
